Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Research Article(ISSN: 2637-6679) 
Antibacterial Activity and Phytochemical Analysis of Aqueous Leaf Extract of Azadirachta Indica on Bacteria Isolated From Cooked Foods (Rice and Beans) Among Street Hawkers Volume 6 - Issue 4
Odeh AP1*, Zainab AB2 and Usman AA3
- 1Nutrition International, PHCDA Dutse, Jigawa State
- 2Department of Microbiology, Sokoto State University
- 3Department of Microbiology, Usmanu Danfodio University Sokoto State
Received:August 25, 2021 Published: September 20, 2021
Corresponding author:Odeh AP, Nutrition International, PHCDA Dutse, Jigawa State
DOI: 10.32474/RRHOAJ.2021.06.000247
Abstract
The present study was carried out to screen the Phytocompounds and as well evaluate the antibacterial activity of the aqueous leaf extracts of the neem tree (Azadirachta indica) on bacteria isolated from prepared spoilt rice and beans. Aqueous extract of leaves of A. indica (Neem) were tested against Staphylococcus gallinarum, Bacillus lentus, Clostridium sordellii, Bacillus firmus and Clostridium botulinum that were isolated from the spoilt cooked rice and Beans. The Neem plants were collected fresh from UDUSOK/permanent site at the Biological garden and transferred to herbarium for authentication before allowing to dry. The activity of the extracts was studied and determined at different concentrations of 100mg/ml, 150g/ml, 200mg/ml and 250mg/ml on the bacteria using agar well-diffusion method. The susceptibility of the bacteria to the extracts was determined by measuring the diameter of inhibition zones formed around the plates. The test analysis showed different zones of inhibition that increased with the increase of the plant extracts concentration on the test organisms. In this study, B. lentus and C. sordellii were susceptible to the extracts at certain concentrations and S. gallinarum were susceptible to the extracts at all concentration while, B. firmus and C. botulinum were resistance to the effect of the extracts at all concentrations used as such there was no zone of inhibitions observed. The results showed that the effectiveness of the extracts was dependent on the concentration used thus the increase of extract concentration increase with the zone of inhibition.
Keywords:Aqueous Extracts; Susceptible; Zone of Inhibitions; Concentration
Introduction
Plants provide an alternative strategy in search for new drugs, there is a rich abundance of plants reputed in traditional medicine to possess protective and therapeutic properties [1]. Bacterial resistance to antibiotics represents a serious problem for clinicians and pharmaceutical industry. Therefore great efforts are being made to reverse this trend, of which one of them is the widespread screening of medicinal plants from the traditional system of medicine hoping to get some newer, safer, and more effective agents that can be used to fight infectious diseases Natarajan et al. [2]. Azadirachta indica is one of such medicinal plants belonging to the Meliaceae family (Mahogany family) and is indigenous to southern Asia. Azadirachta indica, commonly known as neem, has attracted worldwide prominence in recent years, owing to its wide range of medicinal properties and neem has been extensively used in Ayurveda, Unani and Homoeopathic medicine and has become a cynosure of modern medicine. Neem elaborates a vast array of biologically active compounds that are chemically diverse and structurally complex. More than 140 compounds have been isolated from different parts of neem. All parts of the neem tree leaves, flowers, seeds, fruits, roots and bark have been used traditionally for the treatment of inflammation, infections, fever, skin diseases and dental disorders. The medicinal utilities have been described especially for neem leaf Biswas et al. [3]. Neem leaf and its constituents have been demonstrated to exhibit immunomodulatory,anti-inflammatory,antihyper-glycaemic,antiulcer, antimalarial, antifungal, antibacterial, antiviral, antioxidant, antimutagenic and anticarcinogenic properties Talwar et al. [4].
The Neem Azadirachta indica A. Juss [5] is an evergreen robust tree, belonging to the family Meliaceae. It is mostly found in the tropics and sub-tropical region of the world (Africa and Asia). It has medium to large size and have brown to dark grey bark and a dense rounded arrow of pinnate leaves Ogbuewu [6]. The plant has an extensive deep root system which is responsible for their survival in arid and semi-arid area of the world. The chemical constituent of the neem plant is a blend of 3 to 4 actively related compounds, with over 20 lesser ones. Presently over 250 compounds has been identified. The important classes include triterpenoids and limuloids: saladucin, valassin, meliacin, NimbinNimbicin, geducin, Azadirachtin etc. (Koul et al. [7,8]; Uko and Kamal [9]; Lale [10]). Accordingly, all parts of this plant are useful and have been used in treatment of diseases ranging from teeth decay, ulcers, swollen liver, malaria, dysentery, diarrhoea etc. (Ogbuewu, [6]; Allameh et al. [11]; Mossini et al. [12]). Aqueous of Neem leaf extract has a good therapeutic potential as anti-hyper glycaemic agent in IDDM and NIDDM Sonia and Srinivasan [13]. (Abu et al. [14]) suggests that anti-inflammatory effect of Neem extract is less than that produced by dexamethasone. Neem leaves has antibacterial properties and could be used for controlling airborne bacterial contamination in the residential premise, (Saseed et al. [15]; El-Mahmood et al. [16]). The trends in the development of resistance by Microorganism particularly bacteria to modern medicine is of immediate concern, as this makes the disease to be of imminent danger to the populace. Thus, the need arises to determine the phytocompounds present in the Neem tree so as to determine the antibacterial activity on the bacteria associated with spoilt foods.
Materials and Methods
The fresh leaves of the Azadirachta indica plant, was obtained from permanent site of Usmanu Danfodiyo University Sokoto. The plant leaves were taken to Herbarium section in the Biological sciences Department of Usmanu Danfodiyo University Sokoto and were authenticated. It was later transferred to the Microbiology Laboratory of Usmanu Danfodiyo University Sokoto for further analysis. The Fresh leaves were sorted to remove the dead ones, and wash without squeezing to remove debris and dust particles. A large quantity of the leaves were sun-dried for four days. The dried leaves were mill to get a course powder used for the extraction. 24g of the powder was soaked in 250ml of distilled water and the mixture allowed to stand for 24 hours after which muslin cloth was used to filter the plant residues and the filtrate obtained was further purified by filtration through Whatman No 1 filter paper and then screened for its Phytochemical components, the filtrate was then evaporated to obtain the extract (Atata et al. [17]). cooked food (rice and beans,) was kept in a container at room temperature for about 3 days so as to allow spoilage, the sample was homogenize by putting into a sterilized universal bottle containing distilled water and was blended. Serial dilution of the sample was done to obtain 7 dilutions factor (101 to 107), by diluting 1ml in 9 mls of sterile peptone water, first from stock culture, then from subsequent dilutions. Exactly 0.1 ml of 106 and 107 dilution were then inoculated on Nutrient agar using spread plate technique. The petridishes were incubated at 37℃ for 24 hours. After which the colonial characteristics noted and each colonial morphology subcultured to obtain pure isolates.
Gram Staining
A drop of distilled water was placed on the center of a clean glass slide. From the subcultures, a portion from each colony type was picked and emulsified into the drop of water to form a smear using a sterile wire loop. The smear was allowed to dry and was heat fixed. The fixed smear was flooded with Crystal Violet Stain and allowed to stand for 60 seconds and was washed with distilled water. Lugol’s iodine was added and allowed to stand for another 60 seconds and washed with distilled water. This was stained with Acetone for 30 seconds before washing with water. Finally the smear was decolorized with Safranin and rinsed with distilled water. This was done for all the colonies observed. The slide were then allowed to dry and viewed microscopically for morphological characterization of the bacteria colonies using oil immersion objectives lenses (Cheesbrough [18]).
Biochemical Characterization
Catalase Test: A small portion of the bacteria subculture cell was picked using a wire loop and introduced into a drop of hydrogen peroxide on a glass slide. The present of catalyst was observe by which resulting air bubbles indicate a positive catalase while the absent of bubbles indicate negative catalase (Oyeleke and Manga [19]).
Citrate Utilization Test: An inoculum of the isolate was inoculated into the agar and incubated at 37℃ for 48hrs (Cheesbrough [18]). A ready-to-use dehydrated Simmons Citrate Agar was used to prepare slopes of Simmons citrate medium in bijou bottle, according to standard. A sterile wire loop was used to inoculate the slope with a saline suspension of the test of the test organism by streaking over the entered surface of the slant (i.e in a zigzag manner to cover the surface) and then stabbing deep into butt and incubated for 24 to 48hrs. The media was observed for color change (Cheesbrough [18]).
Motility Test: A small portion of the isolate was stab into triple sugar iron (TSI) medium and it was incubated at 370 c for 24 hours. Motility was observed by the spread of the organisms outward of the stabbed area (Oyeleke and Manga [19]).
Indole Production Test : A small portion of the isolate growth was inoculated in 5ml of sterile peptone water enriched with 1% tryptophan and was incubated at 37℃ for 24-48 hours in ambient air and 0.5ml of kovocs reagent was added and shacked gently. In the positive test indole, the presence of red layer at the surface of the test tube indicate positive, while yellow layer at the surface of the test tube indicate negative e.g Klebsiella pneumonia (Oyeleke and Manga [19]).
Urease test: A sterile wire loop was used to incubate the organisms in slant medium in test tube contains area and the indicator phenol red by stabbing through the center of the medium. The test tube was incubated at 37℃ for 24 hours. When the organisms produce urease enzyme, the color of the slant change from light to orange to magenta, it indicates positive while when the organisms produces urease the agar slant and butt remain light orange (medium retairs) original color (Oyeleke and Manga [19]).
Methyl Red Test (MR): A wire loop full of each isolate will be inoculated onto glucose phosphate peptone water medium and then incubate at 370 c for 48 hours. Few drops of methyl red will be added to the culture (Cheesebrough [18]).
Voges-Proskauer Test (VP): A wire loop full of each isolate was inoculated into Glucose Phosphate Peptone Medium and incubated at 37℃ for 48 hours. 5 drops of 40% KOH was added by 15 drops, Naphtol in ethanol was added, shake and place in a sloppy position and examined for 30-60 minutes (Cheesebrough [18]).
Hydrogen Sulphide (H2S): Small portion of isolate was taken with straight wire loop to make a deep inoculation in the H2S medium. The tube was incubated at 37℃ for 24 hours. The present of black precipitate in the medium indicate positive result while absent of precipitate indicate negative result (Ochei and Kolhatkar [20]).
Triple Sugar Iron (TSI): Triple sugar iron was prepared and with a sterile needle the culture from the solid medium was streaked on the surface of the slant and the butt was subbed three times and incubated at 37℃ for 24 hours. Gas formation was determined by the appearance of one or several bubbles. In the butt, vigorous gas formations can result in cracks or it may be pushed from the bottom. TSI glucose fermenters were indicated by yellow color at the butt. If both the butt and slope were yellow, it indicated fermentation of lactose and sucrose. Fermentation of lactose and sucrose but not glucose was detected with red butt and yellow slope (Oyeleke and Manga [19]). Little portion of each isolate was stabbed in to triple sugar iron agar and incubated at 37℃ for 24 hours. Motility was observed by the spread of the organisms outwards from the stabbed line (Ochei and Kolhatkar [20]). Little portion of each isolate was inoculated by streaking and stabbing into triple sugar iron and incubated at 37℃ for 24 hours. Evolution of blackening on the medium indicated a positive test while absence of blackening indicated negative test result (Cheesbrough [18]).
Preparation of the McFarland Scale: 1% solution of sulfuric acid was prepared by adding 1ml of concentrated Sulfuric acid to 99ml of water and agitated. 1% of Bacl2 solution was prepared by dissolving 0.5g of anhydrous Bacl2 in 50ml of distilled water. They were then mixed in the following proportions 0.05/99.5ml, 0.1/9.9ml, 0.2/9.8ml, 0.3/9.7ml, 0.4/9.6ml and 0.5/9.5ml (1% Bacl2 / 1% H2SO4).the tubes were sealed tightly and stored in a dark place, the inoculum suspension was compared with the scale (Cheesbrough [18]).
Antibacterial Activity Assay: The determination of antibacterial activity assay was done using the agar diffusion method (Cheesbrough [18]). The bacteria were each inoculated into sterile nutrient agar and it was incubated at 37℃ for 24 hours. Then the loop of inoculums was transferred into 5ml of nutrient broth and was incubated at 37℃ for 6 hours. Ditch well of 6mm in diameter was made with a sterile cork borer and the inoculum of the test bacteria was spread on the solid plates with the aid of the sterile swab moistened with bacterial suspension. 100mg/ml, 150mg/ ml, 200mg/ml and 250mg/ml of aqueous extract of Azadirachta indica were each poured in the wells respectively. The plates were incubated at 37℃ for 24 hours, the presence or absence of zone of inhibition was observe in millimeters (mm), (Girish and Satish [21]).
Determination of Minimum Inhibitory Concentration (MIC): MIC of the extracts were carried out using the tube dilution technique described by (Cheesbrough [18]). A double fold sterile dilution was made using Muller-Hilton Broth. Equal volume of Muller-hilton broth and extracts were dispensed into sterile tubes. A quantity of 0.1ml of standardized inoculums was added to each test tube which was incubated aerobically at 37℃ for 2hours. A tube with broth and inoculums served as organism control. A tube with broth and extracts served as extract control. The lowest concentration of the extracts which inhibited the microbial growth was recorded as the minimum inhibitory concentration (MIC). Determination of Minimum Bactericidal Concentration (MBC): Sterile Muller-hilton agar plates were inoculated with samples from each of the test tube that showed visible growth from the MIC test. The plates were incubated for 24hours at temperature of 37℃. The lowest concentration of the extracts that yielded no was regarded as the minimum bactericidal concentration (MBC) (Cheesbrough [18]).
Phytochemical Screening
Twenty grams (20g) of neem (Azadirachta indica) leaves was weight on weighing balance and transferred into beaker containing 200ml of distilled water, it was allowed to be soaked for exactly 24hrs in order to determine the presence of phytochemical compounds. The extracts were evaluated for the presence of alkaloids, balsams, flavonoids, anthraquinones, cardiac glycosides, tannis, steroids, saponins and Volatile Oil (Oyeleke and Manga [19]).
Test for Alkaloids: 2ml of extracts was stirred with 2ml of 10% aquences hydrochloric acid. 1ml was treated with few drops of Wanger’ reagent and second 1ml was treated similarly with Mayers reagent. Precipitation was observed for the presence of alkaloids (Harbone et al. [22]).
Test for Volatile Oil: One ml of the extract was mixed with dilute HCL acid. The appearance of white precipitate indicates the presence of Volatile Oil (Evans and Gupta [23]).
Test for Tannins (ferric chloride test): 5% of Ferric chloride solution was added by drop by drop into 2ml of the extracts and immediate dark green color is an evidence for the presence of Tannis (Harbone et al. [22]).
Test for Steroids: 2ml of the extracts was dissolved in 2ml of chloroform and 2ml of Sulphuric acid were carefully poured through the wall of the test tube, the lower layer was formed. A reddish brown color was observed for the presence of steroid (Harbone et al. [22]).
Test for Flavonoids: Three milligrams (3mg) aliquot of the filtrate and one milligram of ten percent (10%) NaOH (Sodium Hydroxide Solution) were added, when yellow colour is developed then it indicates the possible presence of Flavonoids (Oyeleke and Manga [19]).
Test for Saponins: Ten (10) ml of distilled water were added to 0.5cm³ of the extracts, it was shacked vigorously with the test tube for 2minutes. The presence of frothing indicates Saponins presence (Oyeleke and Manga [19]).
Test for Cardiac Glycosides (Keiller killiani’s test): Two ml of 3.5% ferric chloride solution were added and allowed to stand for one minute. One ml of concentrate H2SO4 was carefully pour dawn the wall of the tube so as to form lower layer. A reddish brawn ring when formed at the interface indicate the presence of cardiac glycoside (Oyeleke and Manga [19]).
Test for Anthraquinones: Two (2.0) ml of the aqueous extracts were mixed with 10ml of benzene, and five (5.0) ml of ammonia solution was added and shacked. Presence of pink, red or violet colour in the ammoniac (lower) phase indicates the presence of anthraquinones (Harbone et al. [22]).
Test for Balsams: The extracts were mixed with the 90% volume of ethanol. Two drop of alcoholic ferric chloride solution was added to the extracts. A dark green color indicates the presence of balsams (Oley et al. [24]).
Results and Discussions
In this study, five different bacteria were isolated with respect to the spoilt food although they have a considerable percentage occurences on the spoilt foods. The bacteria identified are B. lentus, B. firmus S. gallinarum C. sordellii and C. botulinum respectively. The occurrence of some of these organisms in the covered spoilt foods might be due to their ability to form spores. However the occurrence of this bacterial isolates is presented in Table 1. The antibacterial activity of aqueous leaf extracts of Azadirachta indica determined at concentrations of 100mg/ml, 150mg/ml, 200g/ml and 250mg/ ml respectively is presented in Table 2. The antibacterial activity of the aqueous leaf extracts against Staphylococcus gallinarum was recorded at concentration of 100mg/ml (12mm), 150mg/ml (13mm), 200mg/ml (15mm) and 250mg/ml (19mm). The activity of the aqueous leaf extracts against Bacillus lentus and Clostridium sordellii was recorded at concentration of 200mg/ml (9mm) and 250mg/ml each. This indicates that from 100mg/ml as the concentration was increased, the rate of the antibacterial activity increases. Uwimbabazi et al. [25] evaluated the antibacterial activity of the aqueous and ethanolic extracts of leaf and bark of A. indica stating that “the bactericidal activity increases with the increase on the extract concentration”, this is also same in the report of Esimone et al. [26], which says that extract of plants inhibit the growth of various microorganisms at different concentrations with significant differences in the diameter of inhibition zones. This disagrees with the report by Rizza et al., (2001) whom according to them there were no significant difference on the effect of different concentrations of the aqueous leaf extracts of A. indica. In this study the antibacterial activity of the aqueous extracts on B. firmus and C. botulinum on the specified concentrationswere 100mg/ml (0,00mm), 150mg/ ml (0,00mm), 200mg/ml (0,00mm) and 250mg/ml (0,00mm) each which shows that they were resistant to the extracts at the concentrations used. This may be as a result of some phytocomponds that were in trace amount in the extracts. (Tayloe et al. [27]) active compounds may be present in an insufficient quantity in extracts to show activity with the concentration employed. The minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) were determined respectively as to determine the minimum concentration of the extracts which is active against the test isolates as shown in Table 3 and Table 4, It was discovered that at concentration of 150mg/ml the MIC was noted on both B. lentus and C. sordellii. While, at 75mg/ml MBC of the extracts was noted on the bacteria. This shows that the leaf extracts kill the organisms at 150mg/ml but, at concentration below 150mg/ml it may only stop the growth but no killing activity. The antibacterial activity of the aqueous leaf extracts may be as a result of presence of phytocompounds found in the extracts, though some of the phytocompounds were found in trace amount as shown in Table 5. The phytocompounds include; Saponins, Flavonoids, Alkaloid, Volatile oil, Cardiac glycoside, Steroids, and Tannins, the presence of these phytocompounds suggests potential for the plant extracts as a source of phytomedicine (Bala [28]). The antibacterial activity is greatly influenced by the presence of Saponins and Flavonoids [29-52].
Table 3: Minimum Inhibitory Concentration (MIC) of an aqueous leaf extracts of Azadirachta indica on Bacillus lentus, Clostridium sordellii and Staphylococcus gallinarum.
Key: - =No Growth; + =Growth Found
Table 4: Minimum Bactericidal Concentration (MBC) of an aqueous leaf extracts of A. indica on S gallinarum, B lentus and C sordellii.
Key: - =No Growth; + =Growth Found.
Table 5: Phytochemical analysis of the aqueous leaf extract of A. indica.
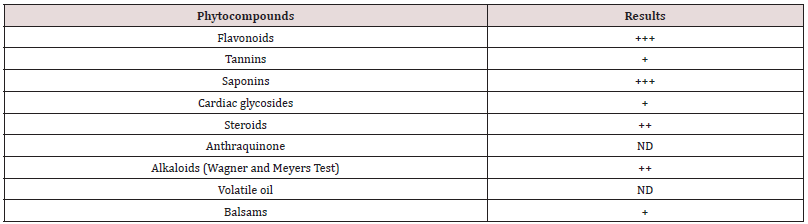
Keys: + = Present in trace amount, ++= Present in moderate amount, +++= Present in high amount, ND= Not Detected
Conclusion
Antibacterial activity of the aqueous leaf extracts of A. indica on both B. lentus and C. sordellii was recorded at concentration of 200mg/ml and 250mg/ml each, and the activity of the extracts was also observed on S. gallinarum at concentration of 100 mg/ ml, 150mg/ml, 200mg/ml, and 250mg/ml, while Bacillus firmus and Clostridium botulinum were resistant at all concentrations used. The extracts have minimum inhibitory concentration (MIC) of 150mg/ml on both B. lentus and C. sordellii.Having an MIC of 75mg/ml on S. gallinarum and MBC of 150mg/ml was noted on the bacteria. The A. indica leaves possess an antibacterial activity due to the presence of bioactive compounds found present even though, some of these compounds were found in trace amount. Thus, Further research is needed to investigate the activity of neem leaf extracts using other solvents to obtain more information of the effectiveness of the plant leaf. It is important to isolate and separate the bioactive compounds responsible for this antibacterial activity using advance scientific techniques and Spoilt food should be discarded not consumed.
References
- Kayode AAA, kayode OT (2011) Some Medicinal Value of Telfairia occidentalis. American journal of Molecular Biology 1: 30-38.
- Natarajan D, Ramachandran A, Srinivasan K. and Mohanasundari C (2003) Screening for antibacterial, phytochemical and pharmacognostical properties of Indigofera caerulea Roxb. Journal of Medicinal Plants Research 4(15):1561-1565.
- Biswas K, Chattopadhyay I, Banerjee RK, Bandyopadhyay U (2002) Biological activities and medicinal properties of neem (Azadirachta indica). Journal of Current Science 82: 1336- 1345.
- Talwar GP, Dhar R, Zhang K, Garg S, Kumar N (1998) Inhibition of the growth and development of asexual and sexual stages of drugsensitive and resistant strains of the human malaria parasite Plasmodium falciparum by Neem (Azadirachta indica) fractions. Ethnopharmacol 61(1): 31-39.
- Del Serrone P, Toniolo C, Nicoletti M (2015) Neem (Azadirachta indica A. Juss) Oil: A Natural Preservative to Control Meat Spoilage. Foods 4(1):3-14.
- Ogbuewu IP (2008) Physiological Responses of Rabbits Fed Graded levels of Neem (Azadirachta indica) Leaf Meal. Thesis, University of Technology. Owerri, Nigeria pp.200
- Koul O, Isman, MB, CM Ketkar (1990) Properties and uses of Neem, Azadirachta indica. Can J Bot 68: 1-11.
- Isman MB, Koul O, Lowrey DT, Arnason JT, Gagnon D, et al. (1990) Development of Neem based In feticide in Canada In: Locke J.C and Lawson R.H (Eds.). proceedings of a workshop on Neem's Potential in Pest Management Programs. USDA-ARS, Beltsville MD ARS 86: 30-32.
- Uko OJ, Kamalu TN (2001) The neem tree – Uses and Potentials. Nigerian Journal of Experimental and Apply Biology 2: 223-239.
- Lale NES, Mustapha A (2000) Efficacy and Acceptability of Neem ( Azadirachta indica A. Juss.) Seed oil and Pirimiphos-methyl for The Control of Callosoburchus Maculatus (F.) (Coleoptera: Bruchidae). Journal of Plant Disease and Protection 107: 399–405
- Allameh A, Razzaghi AM, shams M, Rezaei MB, Jaimand K (2002) Effects of Neem Leaf Extracts On Production of Aflatoxins and Fatty acid Synthetase, Citrate dehydrogenase and Glutathoine Stransferase in A. parasiticus. Journal of Mycopathologia 154: 79-85.
- Mossini SA, deOliveira KP, Kemmelmeier C (2004) Inhibition of Patulin Production by Penicillium Expansum Cultured with Neem (Azadiractha indica) Leaf Extracts. Journal of Basic Microbiology 44(2): 106-113.
- Sonia Bajaj, Srinivasan BP (1999) Investigation into the Anti-diabetic activity of Azadirachta indica. Indian journal of pharmacology 31: 138-141.
- AbuSyed MM, Mamun M, Ur Rashid (2008 ) A comparative study of Anti-inflammatory effect of aqueous extract of Neem leaf and dexamethasone. Bangladesh Journal of Pharmacology 3: 44-47.
- Saseed A Khan, Junaid Aslam (2008) Study on the effect of Neem (Azhadirachta indica) leaves smoke in controlling airborne Bacteria in Residential premises. Current research in Bacteriology1 (2): 64-66.
- EI Mahmood AM, Ogbonna OB, Raji M (2010) The antibacterial activity of Azadirachta indica (Neem) associated with eye and ear infections. Journal of medicinal plant Research 4(14): 1414-1421.
- Atata RF, Sani A, Ajewole SM (2003) Effect of Stem Bark Extracts of Enantia Chloranta on ome Clinical Isolates. Journal of Nigerian Society for Experimental Biology15(2): 84- 92.
- Cheesbrough M (2002) Medical Laboratories Manual for Tropical Countries. Cambridge University Press pp. 479.
- Oyeleke SB, Manga SB (2008) Essential of Laboratory Practical in Microbiology. To best publisher, Minna, Niger state Nigeria. 1st
- Ochei J, Kolhatkar A (2000) Medicinal Laboratory Science Theory and Practice. Tata Mc Graw Hill, India pp: 646-657.
- Girish H, Satish S (2008) Antibacterial Activity of Important Medicinal Plants on Human Pathogenic Bacteria a comparative analysis. World Applied Sciences Journal 5(3): 267-271.
- Harbone CA, Brenner FW, Wells JG, Strockbine NA (1973) Escherichia coli, Shigella, Health 26: 625-630.
- Evans L, Gupta PC (1980) Two new anthraquinones from the seeds of Cassia occidentalis Linn. Cell Molecular and Life Science 30(8): 850-851.
- Oley C, Shanley S, Ratcliffe J, Hockey A, Haan E, et al. (1994) Nevoid Basal Cell Carcinoma Syndrome. 50(3): 282-90.
- Uwimbabazi, F, Uwimana J, Rutanga JP (2015) Assessment of Antibacterial activity of Neem plant (Azadirachta indica) on Staphylococcus aureus and Escherichia coli. Journal of Medicinal plants Studies 3(4): 85-91.
- Esimone CO, Adiukwu MU, Okonta JM (1988) Preliminary Antimicrobial Screening of the Ethanol Extract from the Lichen Usnea subfloridans. 3(2): 99-102.
- Taylor JLS, Rabe T, McGaw LJ, Jager AK, et al. ( 2001) Towards the Scientific validation of Traditional Medicinal Plants . Plant Growth Regulation p.34-37.
- Bala sidi Aliyu (2006) Common Ethnomidicinal Plants of the semi arid regions of West Africa: Their description and Phytochemicals. 1: 82-111.
- Adebayo ES, Samuel TA, Charity DG and Ezekiel BO (2008) A review of Neem Biopesticide Utilization and Challenges in Central Northern Nigeria.
- Badam L, Jashi SP and Bedekar SS (1999) Invitro activity of neem (Azadirachta indica, A Juss) leaf extract against group B coxackievirus National institute of virology, Pune, India 494. Journal of Community Diseases 31(2):79-90.
- Bhatnar D, Zeringue HJJ, McCormick SP (1990) Neem Leaves Extracts Inhibit Aflatoxin Biosynthesis in Aspergillus flavus and Aspergillus parasiticus. Locke Journal of Plant Chemistry and Lawson RH (Eds). proceedings of a workshop on neem's potential in pest management programs. USDA ARS Beltsville 86: 118-127.
- Bhowmik SH, Chattopadhyay, Dasgupta S (2010) Proterozoic Tectonic; An Indian Perspective. Proc Indian National Science and Academic 78: 385-391.
- Cheesbrough M (2004) District Laboratory Practisein Tropical countries, Cambridge University Pres, United Kingdom pp. 382-407.
- El olemy MM, Al muhtadi F T, Afifi AA (1994) Experimental Phytochemistry; A Laboratory Manual. King saud University Press.
- Ganguli S (2002) Neem: A therapeutic for all season, current science. 82(11): pp.1304.
- Gayatri N, Rajani KS (2014) Bio efficacy of Girish K and Shankara Bhat (2008) Neem, A Green Treasure. Electronic Journal of Biology 4(3): 102-111.
- Hoelmer KA, Osborne L, Yokami RK (1990) Effects of Neem Extract on Beneficial Insects in Greenhouse Culture. In: Locke JC and Lawson RH (). proceedings of a Workshop on Neem's Potential in Pest Management Programs. USDA-ARS, Beltsville MD ARS 86: 100-105.
- Jensen JT (2002) Male Contraception.” Current Womens Health Reports. Journal of Medicinal Plants 8: 269-276.
- Kausik B, Ishita C, Ranajit K, Uday B (2002) Biological Activities and Medicinal Properties. Neem (Azmlirachtu iiulica). Journal of Current Science 82(11): 1336-1337.
- Kumar VS, Navaratnam V (2013) Neem (Azadirachta indica): Prehistory to contemporary medicinal uses to humankind. Asian Pacific Journal of Tropical Biomedicine 3 (7): 505-514.
- Larson R (1990) Commercialization of the neem extract margosan-O in a USDA collaboration. In: Proceedings of a workshop on neem's potential in pest management programs. Locke J and Lawson II (), USDA-ARS Beltsville Ml) ARS 86: 23-28.
- Liiulquist K, Adams J, I kill P, Adams 11 (1990) Laboratory and greenhouse evaluations of margosan-O against bifenthrin-resistant and-susceptible greenhouse white flies. Trialeurodcs (llomoptera: Aleyrodidae). In: Proceedings of a workshop on neem's potential in pest management programs. Locke 1 and Lawson R (eds.), USDA-ARS, Beltsville, Ml) 86: 91-99.
- Mohammed B (2005) Interactive Effect of Different Fertilizer Rate, application of Neem Leaf Extract and Benomyl on Yield and Diseases of Cowpea (Unpublished). PGD Crop Production Thesis. Federal University of Technology, Minna Niger State pp.1-34.
- Mukhtar IA (2008) Bioactivity of Neem (Azadirachtaindica) Callus Extract, Omdurman Islamic University Faculty of Science and Basic Medical Science Department of microbiology 2: 3-5.
- Nasir A (2010) Antifungal activity of neem leaf extract on fungal Mycoflora isolated from cowpea (Vigna unguiculata), Usmanu Danfodiyo University, research work.
- Rizza A, Mary LE, Margrett NJ (2001) Antibacterial Effects of Neem (Azadirachta indica ) Leaf Extracts on Staphylococcus aureus.
- Sadre NL, Deshpande VY, Mendulkar KN, Nandal DH (1983) Male Antifertility Activity of Azadirachta indicain Different Species. In Schmutterer, H, and KRS Ascher (eds.) Natural Pesticides from the Neem tree (Azadirachta indica A. Juss) and other tropical plants: Proceedings of the 2nd International Neem Conference. Deutsche Gesellschaft für Technische Zusammenarbeit: Robdorf, Germany.
- Suryawanshi J and Saonere A (2011) Neem-natural contraceptive for male and female an overview, Department of Pharmacy, Government Polytechnic Gadge Nagar, Amravati 444603, India.
- Verpoort F, Tineke V, Vercauteren A, Baeyens W, Vander Weken G, et al. (2002) Application of Romam Spectroscopy in Pharmaceutical Analysis. Journal of Trends in Analytical Chemistry 21(12): 869-877.
- Yaradua AA (2007) Potentials of Biopesticides from Neem tree (Azadiracta indica A. Juss) In Sustainable Pest and Disease Management in Nigeria. Medicinal Plants in Agriculture. Proc.Akure-Humbolt Kellog 3rd SAAT Annual Conference pp. 237-254.
- Yu D, Chen Y, Pan Y, Li H, McCormac, MA, et al. (2008) “Case report: Staphylococcus gallinarum bacteremia in a patient with chronic hepatitis B virus infection”. Annas of Clinical and Laboratory science. 38(4): 4014.
- Zehnder GW, Warthman JW, Locke JC, Larson RH (1990) Activity of Neem Extract and Margosano for Control of Colorado potato beetle in Virginia. In: proceedings of a Workshop on Neem's Potential in Pest Management Programs. USDA-ARS, Beltsville MD ARS 86: 67-75.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)