Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Review Article(ISSN: 2641-1725) 
Investigation on Gastrointestinal Tract: A Review Volume 1 - Issue 4
Amrish Kumar*, Vrish Dhwaj Ashwlayan, Mansi Verma, Vipin Kumar Garg, Anurag, Anjana Sharma, Sameksha Koul, Avnish Kumar Singh, Nitin Sharma, Anoop Kumar, Anuj Kumar, Garima Garg, Shobhit Kumar, Sachin kumar, Nishant Kumar and Satish Kumar Gupta
- Department of Pharmaceutical Technology Meerut Institute of Engineering and Technology, N.H. 58, Delhi-Roorkee Highway, Baghpat, Bypass Road Crossing, Meerut, Uttar Pradesh 250005
Received: August 30, 2018; Published: September 10, 2018
*Corresponding author: (Research Scholar) Amrish Kumar, Department of Pharmaceutical Technology, Meerut institute of engineering and technology, Meerut, N.H. 58, Delhi-Roorkee Highway, Baghpat road crossing, Meerut, Uttar Pradesh 250005, India
DOI: 10.32474/LOJMS.2018.01.000116
Abstract
The gastrointestinal (GI) tract is composed of organs and tissues that have diverse forms and functions. It includes the esophagus, stomach, small intestine, large intestine, colon, rectum, biliary tract, gallbladder, liver, and pancreas. Despite the rapid proliferation of technology for the diagnosis of digestive diseases, the patient history and physical examination still hold central roles. When combined with a thorough patient history and physical examination, diagnostic procedures are essential in the evaluation of GI disorders. This review describes the most commonly used tools available in clinical practice to evaluate patients with GI diseases.
Keywords: Gastrointestinal Tract; Gallbladder; Digestive Disease; Pancreas
Introduction
Symptoms of gastrointestinal dysfunction
A variety of symptoms can arise from GI dysfunction. Common GI symptoms include heartburn, abdominal pain, dyspepsia, nausea, vomiting, diarrhea, constipation, and gastrointestinal bleeding. Signs and symptoms of malabsorption, hepatitis, and GI infection are also commonly seen. The next sections describe methods that are commonly used to assess patients with GI complaints.
Patient history
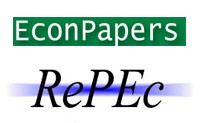
A comprehensive patient history is the cornerstone in the evaluation of a patient with digestive complaints. A clear, detailed, chronologic account of the patient’s problems should be ascertained. This account should include the onset of the problem, the setting in which it developed, and its manifestations. The onset of the problem often provides important information that helps to confirm diagnosis. For example, biliary pain, such as that encountered with symptomatic gallstone disease, typically evolves over minutes and lasts for hours, but pain caused by pancreatitis evolves over hours and lasts for days. The setting is always relevant as it provides clues to the possible origin of the disorder. For example, is the patient an alcoholic (liver disease, esophageal varices, or pancreatitis)? Does the patient have severe atherosclerosis (mesenteric ischemia)? Is the patient immunosuppressed (opportunistic infection)? Also aiding in the differential diagnosis is identification of factors that alleviate or exacerbate the principal symptom. For instance, ingesting a meal often relieves the pain of duodenal ulcer, but worsens that of gastric ulcer. The health care professional should ask questions that address the potential etiologic possibilities, including motility disorders, structural diseases, malignancies, infections, psychosocial factors, dietary factors, and travelassociated diseases [1,2]. Questions concerning past medical and family history detailing illnesses, surgeries, injuries, and habits are extremely valuable. Because many drugs have been reported to cause GI injury, a patient’s medication history is also vital. Table 1 revealed, those drugs which cause gastrointestinal injury.
Physical Examination
Because the organ systems of the body interact and may provide important data needed for diagnosis, it is necessary to perform a thorough physical examination.3 A global evaluation of the patient should be performed with notable attention to appearances and vital signs because they may suggest clues to the patient’s overall condition and stability. Careful examination of the abdomen is also an essential part of the work-up. Examination of the abdomen is classically approached by inspection, auscultation, percussion, and palpation. Inspection of the abdomen may reveal scars, hernias, bulges, or peristalsis. Auscultation is mainly focused on analysis of bowel sounds and identification of bruits. Percussion of the abdomen allows for detection of tympany, measurement of visceral organs, and detection of ascites. Palpation may allow the clinician to identify tenderness, rigidity, masses, and hernias. A digital rectal examination is used to detect masses, tenderness, and assess muscle tone. Stool on the examiner’s glove obtained during rectal examination is often subjected to hemoccult testing for the indirect detection of occult blood [3].
Laboratory and Microbiologic Tests
Laboratory and microbiologic tests may be used to (a) assess organ function, (b) screen for certain GI disorders, and (c) evaluate the effectiveness of therapy. To achieve an accurate diagnosis and provide the best care, it is important to assess the patient’s fluid and electrolyte status, nutritional status, and abdominal organ function. A serum chemistry panel provides clinicians with valuable information. For example, serum creatinine (SCr) and blood urea nitrogen (BUN) are often used as a measure of hydration status, as well as serving as indicators for renal function. Elevations in SCr and BUN may be indicative of renal dysfunction or dehydration, and bleeding from the GI tract may lead to elevations in BUN. Albumin levels can be used to assess the patient’s nutritional and hydration status and provide information concerning hepatic and renal function. Specifically, low albumin may be indicative of malnutrition, hepatic dysfunction, nephrotic syndromes, or protein-losing enteropathies such as Crohn’s disease and ulcerative colitis. Serum measurements of sodium, chloride, and potassium are useful to determine electrolyte abnormalities associated with diarrheal illnesses. A complete blood count (CBC) helps to provide information concerning infection, malignancy, bone marrow suppression, anemia, and blood loss [4] Specific laboratory blood tests are used as screening tools for certain GI disorders. For example, measurements of serum aspartate transaminase (AST) and alanine transaminase (ALT) are elevated in most diseases of the liver, and serum alkaline phosphatase and bilirubin are often elevated in hepatobiliary disorders. Because prothrombin time is related to hepatocyte synthesis of vitamin K–dependent clotting factors, it serves as an indirect measure of hepatic function. When evaluating patients with suspected pancreatitis, serum and urine measurements of amylase and lipase are important, because these will be elevated in most patients with acute pancreatitis. Microbiologic studies are useful in evaluating patients with unexplained diarrhea, abdominal pain, and suspected GI infections. Microbiologic studies of the stool may be used to detect the presence of bacteria and parasites. Pathogens most often responsible for infectious diarrhea and enteritis include bacteria such as Shigella, Salmonella, Escherichia coli, and Yersinia; viruses such as cytomegalovirus, especially in AIDS patients; and parasites such as Entamoeba histolytica and Giardia lamblia [5]. Because Helicobacter pylori is a significant factor associated with peptic ulcer disease and gastritis, identification of this organism is critical in evaluating patients experiencing dyspepsia
Diagnosis
The patient history, physical examination, and routine laboratory tests are extremely useful in establishing a diagnosis, but frequently a more specific study is required to confirm or disprove a clinical suspicion. The most appropriate diagnostic test depends on the anatomic region involved, the suspected abnormality, patient preference, the patient’s overall condition, and clinical manifestations of the patient. The next sections outline the most frequently used diagnostic studies and procedures and their roles in evaluating the GI tract.
Radiology
Radiologic procedures rely on the differential absorption of radiation of adjacent tissues to highlight anatomy and pathology. Radiologic procedures important in evaluating the GI tract include plain radiography, upper GI series, lower GI series, and enteroclysis [6,7].
Plain Radiography of The GI System
Radiographic evaluation of the GI tract often starts with plain films of the abdomen, which are straightforward, uncontrasted radiographs. Specific abdominal structures that may be identified include the kidney, ureters, and bladder (KUB); esophagus; stomach; intestine; stones; and vessels. Plain films are often used to evaluate abdominal pain. Clinicians frequently employ plain radiographic fluoroscopy to guide and position other instruments that are used to evaluate and treat GI disorders; an example is the manipulation of dilation devices to treat esophageal strictures. Bowel obstruction and perforation are especially well identified by this technique.
Contrast Agents
Many different types of contrast agents are available. Two types of contrast agents commonly used to enhance visualization of the GI tract are barium sulfate and aqueous iodinated compounds. Barium sulfate is the contrast agent of choice for studying the esophagus, stomach, and intestine, except in special clinical situations.7 Barium sulfate is not generally absorbed, and constipation is the most frequent adverse effect reported with its use. Two widely used iodinated contrast agents for visualizing the GI tract are diatrizoate, meglumine and diatrizoate sodium. Unlike barium, these agents are relatively nontoxic if inadvertently introduced into the peritoneal cavity; therefore the main indication for use of iodinated agents in GI radiography is for suspected bowel perforation. Because iodinated contrast agents are hyperosmolar, they possess the potential to cause severe diarrhea, dehydration, and electrolyte imbalances. Nephrotoxicity associated with iodinated contrast agents may occur and is generally self-limited [8]. Allergies and hypersensitivity reactions such as rashes associated with contrast agents are possible and should be monitored and treated Accordingly.
Upper GI Series
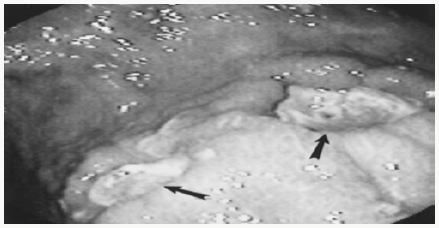
The upper GI series refers to the radiographic visualization of the esophagus, stomach, and small intestine. Patient preparation for an upper GI usually consists of instructing patients to refrain from eating or drinking 8 to 12 hours prior to testing, thereby allowing the upper GI tract to empty. A contrast agent such as barium sulfate is administered to the patient at the beginning of the study. The observed swallowing of the contrast agent permits visualization and monitoring of esophageal structural and motor functions. This phase of the procedure is most often referred to as a barium swallow. As the contrast medium flows into the stomach and small intestine, several regional radiographic films are taken in order to inspect these areas. This tracking of contrast agents through the small intestine is referred to as the small bowel followthrough. The upper GI series with the small bowel follow-through includes the examination of the esophagus to the distal end of the small intestine, and is useful to evaluate and detect obstructions, tumors, ulcers, and abnormal intestinal loops. The upper GI series with small bowel follow-through commonly uncovers gastric cancer, peptic ulcer disease, esophagitis, gastric outlet obstruction, and Crohn’s disease (Figure 1) revealed upper gastrointestinal tract with Crohn’s disease.
Figure 1: Upper GI series with small bowel follow-through demonstrating narrowed distal terminal ileum and separation of small bowel loops (arrow). These findings are consistent with Crohn’s disease.
Lower GI Series
The lower GI series is used to examine the colon and rectum. Patients complaining of lower abdominal pain, constipation, or diarrhea are often referred for a lower GI series. Before the procedure the colon is prepared by instructing the patient to refrain from eating or drinking 8 to 12 hours before the procedure, and by administering bowel cleansing agents such as bisacodyl, magnesium citrate, magnesium hydroxide, or polyethylene glycolelectrolyte solution. During a lower GI series, a barium sulfate enema is given to contrast the terminal large intestine and rectum. The lower GI series is useful to detect and evaluate enterocolitis, obstructions, volvulus, and mucosal and structural lesions. The lower GI series is commonly used to diagnose Crohn’s disease, ulcerative colitis, colon cancers, and diverticulitis.
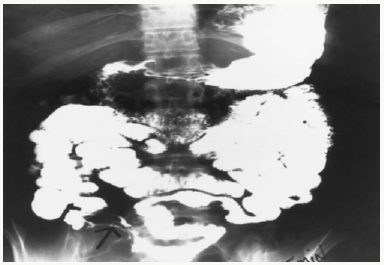
Small Bowel Enteroclysis
Enteroclysis or small bowel enema refers to the technique of direct small bowel introduction of a contrast agent through a tube inserted through the patient’s mouth or nose. Intermittent radiographic films are taken of the small bowel as the contrast agent flows distally (Figure 2) revealed normal small bowel enteroclysis. Because enteroclysis provides detailed imaging, it is an accurate method for evaluating the small bowel and for detecting small mucosal lesions that may be overlooked on the traditional small bowel follow-through [9]. Methylcellulose is used to enhance the detail of the small intestine in enteroclysis, thereby improving visualization. Patient preparation for this procedure involves instructing patients to refrain from eating or drinking 8 to 12 hours before testing and administering bowel-cleansing agents. The most frequent disorder evaluated by enteroclysis is obscure GI bleeding.
Figure 2: Normal small bowel enteroclysis. Contrast agents are instilled into the small bowel to highlight tumors, strictures, or other lesions. In this image, one can identify the normal circular folds.
Ultrasonography
Ultrasonography provides images of deeper structures such as the gallbladder, liver, pancreas, and abdominal wall. The clinician is able to image slices of the GI tract by directing a narrow beam of high-energy sound waves into the body and recording the reflections from the various organs and structures. Because ultrasonography is noninvasive, relatively inexpensive, requires no ionizing radiation, and can be performed with a portable unit, it is a well-accepted and useful technology. It accurately depicts gallstones and gallbladder, and hepatobiliary and pancreatic diseases. Figure 3 revealed abdominal ultrasound demonstrating a chronic pancreatic pseudocyst. When combined with Doppler technologies, ultrasonography may image GI vascularity. Ultrasonography is limited by the presence of bowel gas and excessive amounts of body fat [10,11].
Radionuclide Imaging
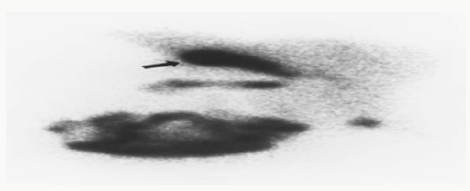
Radionuclide imaging involves intravenous injections of a radiopharmaceutical imaging agent and the use of a computerized detection camera to gather images. Although the choice of a radiopharmaceutical agent depends on the specific organ or function being studied, the most commonly used agent is technetium (Tc-99m) tagged to a carrier molecule. Radiographic imaging is useful to visualize the liver and spleen (liver-spleen scan), bile ducts, gallbladder (HIDA [hepatoiminodiacetic acid] scan), and gut (bleeding scan). Cysts, abscesses, tumors, and obstructions are detected and displayed as areas of differential uptake of radioactivity (Figure 4). Radionuclide bleeding scans may detect hemorrhages and may assist in localization.
Computed tomography
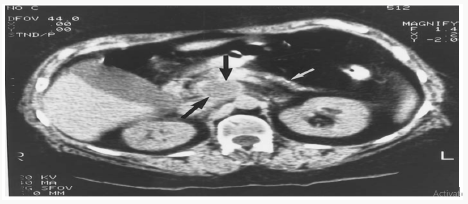
Computed tomography (CT) or computed axial tomography (CAT) scans provide detailed images of the GI system in which transverse planes of tissue are swept by a radiographic beam and a computer analysis of the variance in absorption produces a precise reconstructed image of that area. Contrast agents may be added in a CT procedure to illuminate specific hollow structures and vascularity of the GI tract. The abdominal CT displays organs from the diaphragm down to the pelvic brim, and is especially valuable for detecting GI diseases of the liver, pancreas, spleen, and colon. Patient preparation for CT includes refraining from eating or drinking for a minimum of 4 hours before the test. The remarkable detail that CT offers in imaging organs and tissues adds to its popularity for evaluation of the GI system. CT is useful in the identification of liver cancer, pancreatitis, pancreatic cancer, intraabdominal abscesses, and cysts (Figure 5). Unlike ultrasonography, patient body size or the presence of gas does not limit the quality of imaging with CT.
Figure 5: CT scan of the abdomen showing pancreatitis with calcification (white arrow) and pancreatic pseudocyst (black arrows).
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) places the patient in close proximity to a high-strength magnetic field through which pulses of radiofrequency radiation are projected, thereby exciting the nuclei of hydrogen, phosphorus, oxygen, and other elements. The radiofrequency signals are manipulated and recorded by a computer, and a two-dimensional image representing a section of the patient is produced. MRI has greater sensitivity to identify liver tumors than ultrasonography, CT, or radionuclide imaging. Although currently MRI is not as popular as other imaging techniques because of limited availability, expense, and problems associated with the use of powerful magnetic fields, its use is predicted to increase in the future.
Endoscopy
Refinement in optical engineering and fiber optics has made possible the development of the endoscope, which has revolutionized the management of GI disorders. An endoscope is an illuminated optical instrument designed to inspect the interior of the GI tract. Endoscopes enable the practitioner to inspect intraluminal mucosal lesions and to obtain biopsies and washings for cytology studies. Upper GI tract endoscopy (esophagogastroduodenoscopy) is capable of inspecting the esophagus, stomach, and proximal small bowel. Lower GI tract endoscopy of the rectum and colon may be accomplished by colonoscopy or sigmoidoscopy. Endoscopy can also be used to perform many therapeutic procedures. Preparation for endoscopic examinations includes instructing patients to refrain from eating or drinking 8 to 12 hours prior to the endoscopic procedure. Bowel cleansing is necessary for colonoscopy and sigmoidoscopy. Topical pharyngeal anesthetics such as viscous lidocaine or benzocaine usually improve patient acceptance of the upper endoscopic tube. Intravenous sedating agents such as meperidine hydrochloride, diazepam, lorazepam, and midazolam hydrochloride are among the most common agents used to induce “conscious sedation” minutes prior to the endoscopy. These sedating agents tend to improve patient acceptance and ease of the procedure. With the development of flumazenil, a benzodiazepine antagonist, the use of benzodiazepines for mild sedation during GI procedures has increased. In addition, antimuscarinic agents such as atropine sulfate are occasionally used for their cardiovascular effects, such as increasing a patient’s heart rate, or for their antispasmodic effects, such as reducing duodenal and colonic motility. Because of its effectiveness at reducing bowel motility, glucagon is also often used. Endoscopy is contraindicated for patients with severe respiratory or cardiac failure, and for patients with suspected perforated viscera. The most commonly used endoscopic studies are upper endoscopy, colonoscopy, sigmoidoscopy, and endoscopic retrograde cholangiopancreatography.
Esophagogastroduodenoscopy
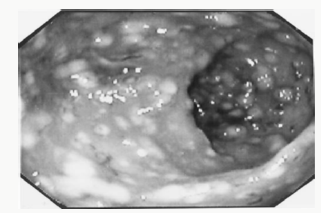
Esophagogastroduodenoscopy (EGD) is used to examine the esophagus, stomach, and duodenum. Patient preparation for EGD includes fasting for 6 to 8 hours prior to the procedure and the administration of sedatives and topical anesthetics. Common indications may be either diagnostic or therapeutic in nature, and include evaluating suspected upper GI bleeding, obstructions, upper abdominal pain, persistent vomiting, and radiographic abnormalities [12]. EGD commonly uncovers peptic ulcers and other lesions (Figure 6).
Colonoscopy
Colonoscopy permits direct examination of the large intestine and rectum. To prepare for colonoscopy, the patient should fast for about 8 hours prior to the examination, and bowel cleansing should be completed. Agents such as midazolam and meperidine are usually given to produce conscious sedation. Similarly to upper GI endoscopy, indications for lower GI endoscopy can be either diagnostic or therapeutic in nature, and include evaluation and detection of abnormalities visualized by radiography, as well as GI hemorrhage, colonic lesions, volvulus, ulcerative colitis, Crohn’s disease, diverticulitis, and excision of colonic polyps [13].
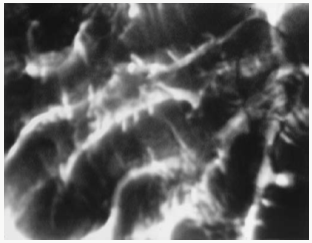
Figure 7: Sigmoidoscopic photograph revealing the lightraised lesions of antibiotic-associated pseudomembranous colitis.
Sigmoidoscopy
Sigmoidoscopy is used to evaluate the sigmoid colon and rectum (Figure 7). Flexible sigmoidoscopy has virtually replaced rigid sigmoidoscopy because of increased patient comfort and superior performance. The major indication for this examination is to evaluate symptoms related to the colon or rectum, and to conduct screening of asymptomatic patients for colon polyps or cancer. Patient preparation involves instructing patients to abstain from eating or drinking 8 to 12 hours prior to the procedure and administering bowel-cleansing agents. Anoscopy is especially useful in evaluating the anus. The major indications for anoscopic examination include symptoms related to the anus and rectum, such as bleeding, protrusions or swelling, pain, and severe itching. Patients undergoing sigmoidoscopy or anoscopy generally do not require sedation.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP is an important procedure that is used to evaluate and treat diseases of the biliary tree and pancreas. By injecting contrast agents through a catheter swallowed and acts as an endoscope. While the video capsule travels naturally through the digestive tract, images are transmitted to a recording device. Patients return the recording device to the practitioner so that the images can be downloaded to a computer and evaluated. Eventually, the camera is naturally excreted and not retrieved [14].
Conclusion
Evaluation of the GI tract begins with a careful history and comprehensive physical examination. It then proceeds in a deliberate and thoughtful manner to establish the correct diagnosis and appropriate management. Laboratory and microbiologic tests, radiography, ultrasonography, computed tomography, radionuclide scanning, magnetic resonance imaging, arteriography, endoscopy, esophageal manometry, pH monitoring, endoscopic ultrasonography, and laparoscopy have definite roles in diagnosing and evaluating GI disorders.
References
- Kearney DJ Approach to the patient with gastrointestinal disorders (2003) Diagnosis &Treatment in Gastroenterology. Lange Medical Books/McGraw-Hill, New York, USA.
- Isselbacher KJ, Podolsky DK Approach to the patient with gastrointestinal disease (1991) Harrison’s Principles of Internal Medicine., McGraw-Hill, New York, USA.
- Bates B.A. Guide to Physical Examination (1994) Lippincott, Philadelphia, USA.
- Jacobs DS, Demott WR, Finley PR Laboratory Test Handbook (1994) Lexi-Comp, Cleveland.
- Guerrant RL. Principles and syndromes of enteric infection (1990) Principles and Practice of Infectious Diseases., Churchill Livingstone, New York, USA.
- Novelline RA Squire’s Fundamentals of Radiology (1997) Harvard University Press, Cambridge, USA.
- Cohen AJ. Radiologic general diagnostic and imaging studies of the small and large bowel (1994) Principles and Practice of Gastroenterology and Hepatology. CT, Appleton & Lange, Stamford.
- Smith CR, Petty BG Specific complications of medical management (1988) The Principles and Practice of Medicine. CT, Appleton & Lange, Stamford, USA.
- Miller RE, Sellink JL (1979) Enteroclysis: The small bowel enema How to succeed and how to fail. Gastrointest Radiol 4(1): 269-283.
- Friedman LS, Needleman L. Hepatobiliary imaging (1991) Harrison’s Principles of Internal Medicine., McGraw-Hill, New York, USA.
- Wall SD (1996) Diagnostic imaging procedures in gastro-enterology. Cecil Textbook of Medicine. Saunders, Philadelphia, USA.
- Sartor RB Upper gastrointestinal endoscopy (1993) Manual of Gastroenterologic Procedures. Raven, New York, USA.
- Hay DW, Onion SK (2002) Blackwell’s Primary Care Essentials: Gastrointestinal and Liver Disease. Blackwell Science, Malden.
- News from Mayo Clinic in Jacksonville. Capsule endoscopy goes where few endoscopes have gone before, 2002-2003.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...