
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Case report(ISSN: 2641-1687) 
Diagnosis of Unintentional Urinary Catheter Misplacement in Ureter by Ultrasound Imaging: Report of Two Pediatrics Cases Volume 4 - Issue 4
Kajal Patel1*, Nitin A Patel2, Harsh C Sutariya1 and Shruti P Gandhi3
- 1Associate Professor, Department of Radiology, G. R. Doshi and K. M. Mehta Institute of Kidney Diseases and Research Centre (IKDRC)-Dr. H.L. Trivedi Institute of Transplantation Sciences (ITS), India
- 2Department of Radiology, Surym –The World of Imaging centre, Shivranjani crossroads, India
- 3Professor and Head of department, Department of Radiology, G. R. Doshi and K. M. Mehta Institute of Kidney Diseases and Research Centre (IKDRC)-Dr. H.L. Trivedi Institute of Transplantation Sciences (ITS), India
Received: September 11, 2023; Published: September 21, 2023
Corresponding author: Kajal N. Patel, Associate Professor, Department of Radiology, G. R. Doshi and K. M. Mehta Institute of Kidney Diseases and Research Centre (IKDRC)-Dr. H.L. Trivedi Institute of Transplantation Sciences (ITS), Ahmedabad, Gujarat, India
DOI: 10.32474/JUNS.2023.04.000196
Abstract
Foley’s catheterization is a widely done clinical invasive procedure. It is a comparatively safe procedure with minimal complication rate. Normally the foley’s catheter tip resides in the urinary bladder. Unintentional misplacement of catheter into ureter is extremely rare possibility and only 27 cases reported worldwide till date. It can occur even in patients with no definite risk factors. It can lead to many complications like infection, bleeding, ureteric obstruction, and ureteric injury/rupture. Presentation may vary from persistent urine leakage around a urethral catheter, groin pain, back pain and even can be asymptomatic. It is more common in females. Routine ultrasound imaging after catheterization is not advised routinely but it is necessary when clinical suspicion arises inform of inadequate drainage of urine or discomfort/pain. Other imaging modalities can be performed to evaluate associated complications. Physicians should take care to follow the basic principles of catheterization even if the procedure is considered simple and easy to perform to avoid such complication. A multidisciplinary approach is required to manage this type of complication.
Keywords: Foley’s catheter; unintentional misplacement; urinary bladder; ultrasound
Introduction
Per urethral urinary bladder catheterization is the widely practiced and comparatively safe urological outpatient procedure; routinely performed in many hospitals with a low complication rate. In most cases, this is uneventful with the tip of Foley’s balloon catheter residing within the urinary bladder. However, it is not exempt from complication. The occurrence of unintentional misplacement of catheter into ureter is extremely rare but possible occurrence and only 27 cases reported worldwide till date [1-4]. The mechanism of such misplacement is unclear, but it can lead to complications such as infection, bleeding, ureteric obstruction with hydronephrosis, ureteric injury or even ureteric ruptures with some frequency, but serious complications like bladder perforation and recto vesical fistula rarely occur but has been reported in past [5]. Presentation may vary from persistent urine leakage around a urethral catheter, groin pain, back pain and even can be asymptomatic. It is more common in females. Herein we present two such cases of unintentional urinary catheter misplacement into ureter in pediatric patients presented with urosepsis at our healthcare institute. The purpose of this report of cases is to suggest the possible reasons for this rare occurrence, what measures should be taken to prevent this, imaging characteristics, treatment and to review the literature. Observation of such two cases show that unusual complications can occur in the most common procedures.
Case Presentation
Case 1
An 11-year-old female presented with foley’s catheterization which had been placed outside several hours prior to her presentation at our institute. Patient had history of fever, decreased urine output and generalized anasarca for 15 days. Her past medical history was not significant. The vital signs were unremarkable at the time of presentation. Laboratory reports were significant for leukocytosis (White blood cells of 33.20x1000/mm3) and elevated high sensitivity C Reactive Protein (HS CRP) of 160.34mg/ dl. Elevated Blood Urea nitrogen (BUN) and S. Creatinine were 224mg/L and 9.55mg/L respectively noted. The rest of laboratory investigations were normal in limit. So immediate Ultrasound was advised, and patients came to our radiology department for evaluation of urosepsis.
USG abdomen showed absent right kidney with normal size left kidney with moderate hydronephrosis and hydroureter. Her urinary bladder was empty with absence of foley’s catheter balloon in ultrasound (Figure 1). Inflated Foley’s catheter balloon was visualized in dilated left upper ureter 5 cm distal to pelvic ureteric junction. Isoechoic debris is also noted in left upper ureter (Figure 2). The malpositioned foley’s balloon was subsequently urgently removed by pediatric nephrologist simply by pulling back after balloon deflation without any immediate complication. Shortly following the procedure, the patient’s oliguria resolved to some extent. A follow up ultrasound showed persistent hydronephrosis and hydroureter in left kidney possibly due to poorly functioning solitary kidney.
Figure 1: Ultrasound image (A) minimal distention of urinary bladder with absent foley’s catheter balloon (B) Moderate hydronephrosis in left kidney.
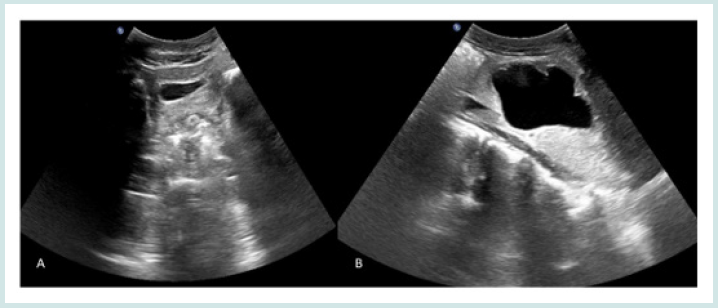
Figure 2: Ultrasound image (A) foley’s catheter with balloon in left proximal ureter (B) debris within ureter proximal to foley’s catheter balloon.

Case 2
A 7-year-old female is a known case of chronic kidney disease with bilateral hydronephrosis and hydroureter. Patient was a known case of cleft palate and her 2D Echo showed small patent ductus arteriosus (PDA). Her Micturating cysto-urethrogram (MCU) Study was done in the past which was negative for vesico-ureteric reflux (VUR). Patient presented with fever and pain in urology department of our institute. Her laboratory investigations showed leukocytosis (White blood cells of 27.0x1000/mm3) and high sensitivity C Reactive Protein (HS CRP) of 18.0mg/dl. Her S. Creatinine level was 4 mg/dl. The rest of laboratory reports were within normal limit. So, the diagnosis of this case was acute on chronic kidney disease secondary to urosepsis. Bilateral PCN diversion and urinary bladder catheterization were done. Ultrasonography (USG) was advised for further workup.
Findings were gross hydronephrosis with hydroureter on either side, left renal stone, distended urinary bladder with absent foley’s catheter balloon. A catheter balloon was found in right lower ureter (Figure 3). Urology residents found resistance at the time of removal of misplaced catheter. So, the patient underwent the urethroscopy for the same. Urethroscopy finding were retained foley’s catheter balloon in right lower ureter with wide right ureteric orifice below bladder neck. During urethroscopy foley’s catheter balloon was deflated by needle puncture and tip of foley’s brought out by forceps. The remainder of the patient’s hospitalization was uneventful. Ultrasound done one day later showed catheter in right place with no definite abnormal findings except bilateral hydronephrosis. Patient underwent left uretero-ureterostomy and right ureteric reimplantation after 3 months. After several days of follow up, we observed no definite related symptoms of this event.
Discussion
Foley’s catheterization is a widely performed clinical outpatient procedure and is considered comparatively safe. But it can be burdensome for a variety of reasons. Iatrogenic trauma during catheterization via urethra can occur inform of formation of a false passage or stricture urethra. However, this type of trauma is very rare with an overall incidence of 0.3% [6]. Catheter related serious complications rarely occur, however infection, inflammatory reactions, bleeding, urethral injury, catheter malfunction, false route and catheter balloon inflation into urethra can be happened [7].
Risk factors
There are few risk factors for unintentional placement of urethral catheter into ureter :- female sex, neurogenic bladder, sensory disorder, history of bladder surgery, empty bladder catheterization and patulous ureteric orifice. Female urethra is short so catheter can easily misdirect into ureter. Pain during catheter misplacement cannot be experienced by patients in case of sensory disorder. Chronic urinary catheterization also leads to misdirection of catheter into ureter; possible reasons for that are 1. Their bladder tends to become contractile (as anatomical relationship between bladder neck and ureteric orifice becomes altered) so it is easier for catheter to enter ureter 2. regular catheter change has more opportunities to be inadvertently placed in ureter 3. neurogenic bladder cases have vesico ureteric reflux with patulous ureteric orifice which are easier for the tip of catheter to enter ureter [8].
Presentation
Patients may present with abdominal or flank pain, pericatheter urine leakage, blockage, catheter expulsion and bleeding.
Imaging
On imaging, a misplaced catheter would have a similar appearance if placed in bladder, but the catheter balloon will be seen along the course of a ureter. Other findings would be according to associated complication the patient has sustained at time of presentation. Diagnosis can be used using ultrasonography, CT scan, MRI, cystoscopy, X ray Abdomen and X rays studies with contrast (intravenous urography, retrograde pyelography or cathtereography).
A spherical hypoechoic/anechoic (if inflated with water) foley’s balloon can be visualized in the abdomen on ultrasound imaging. It is also operator dependent and based on used technique. Proximal hydroureter and hydronephrosis may be seen often due to ureteric obstruction. Urine jet may be visualized with extravasation of urine from injured ureter in case of ureteric rupture. Comet tail artifacts due to air may be seen in pelvic calyceal system or in area of rupture. On CT scan, foley’s balloon appears as a spherical hypodense lesion with water attenuation along the course of ureter. Hydroureter and hydronephrosis is also seen if it present. Urine collection (either of water density or mixed density if associated with blood) will be seen in areas of rupture and possibly in dependent regions of the pelvis. In excretory phase of CECT extravasation of contrast in region of rupture is noted. X RAY abdomen may show misplaced Foley’s balloon shadow along the expected course of ureter instead of in the bladder. If hydronephrosis is present in kidney renal shadow also appeared to be enlarge.
An X ray abdomen standing, or decubitus view may show tiny amount of intraperitoneal free air. On MRI, misplaced foley’s balloon appears as a spherical hyper intense structure in a ureter on T1 weighted imaging. Hydronephrosis appears as hyper intensity of collecting system on T2 weighted imaging, increased signal intensity on diffusion weighted imaging and decreased apparent diffusion coefficient [9]. Extravasated urine appears as T2 hyper intense fluid collection in region of rupture or into pelvis in case of ureteral rupture. The first method to confirm the location of catheter and its balloon is ultrasound imaging of bladder but the technique of choice is CT SCAN to evaluate possible complication and the need for subsequent intervention [10]. As foley’s catheter has unique appearance and seen along course of ureter with obstructive changes proximally, there are no other diagnostic considerations which could create a similar radiological finding. Thus, differential diagnosis has been limited to single diagnosis only.
Measures to be taken to prevent misplacement: Catheter positioning is a basic and important procedure before balloon inflation. To maintain the catheter in place foley’s balloon should be inflated with 10cc sterile water. First one should inflate the balloon with 3 cc of water to confirm the catheter balloon position and then pull down to neck of urinary bladder, once confirmation achieved then rest of 7cc inflation should be done. After this procedure, watch for urine drainage from catheter, if free flow of urine is visualized then consider that the catheter is in correct location [11]. In oliguric and anuric patients correct catheter positioning should be confirmed by irrigation and fluid inhalation before complete balloon inflation [12].
Patients experience pain if the foley’s balloon is not in proper place. So, the history of the patient during catheterization is also important to check the status. Tugging on catheter after balloon inflation is also helpful to avoid misplacement. As misplacement of catheter into ureter can occur either during the initial introduction of device or after subsequent migration, monitoring of urine outflow at time of catheter placement and also on a continuing basis to watch for migration should be done. Short tip catheter should be used in neurogenic bladder cases to reduce the misplacement. As these cases has more chances of inadvertent placement.
Treatment
There are a number of potential techniques to manage this scenario. Misplaced catheters can be removed by using manual syringe aspiration and deflating it. Slow deflation or passive deflation is appropriate to minimize balloon cuffing or entrapment. Catheter can be divided with scissors or cutting off the inflation valve would automatically deflate the balloon in case above methods fail. If non-deflation of balloon persists once the balloon channel has been cut, endoscopic assessment is recommended. Injecting more fluid within the balloon port until the balloon bursts or using solutions such as mineral oil to dissolve the balloon is also another approach to deal with misplaced catheter. However, in those case careful inspection of balloon is required to ensure that there are no retained particles. There are some reasons for non-deflation of misplaced balloon catheter. They are external compression on balloon port lumen by ureter, primary catheter failure, crystallization in balloon, catheter can be folded upon itself within ureter, asymmetric catheter balloon (with respect of body and lumen of catheter) inflation causing kinking or twisting of catheter. These did not allow any fluid or a guide wire to be passed through the inflation port. According to some past studies, about 20 % of the balloon in the 26 cases of catheter misplacement into ureter have failed to deflate. This suggests that misplaced balloons may make deflation more difficult.
It is essential to explore the cause by imaging study prior to removal and real time manipulation using ultrasound device or fluoroscopy. Both ureteroscopes and cystoscopes provides a clear view of position of catheter. The use of guide wires down the inflation port to burst the balloon with biopsy forces, electrodes, and laser fibres (HO: YAG Laser holmium yttrium aluminum garnet laser) can be utilized. Needle puncture with a palpable balloon through the urethra or vagina or if needed under ultrasound guidance can be utilized for deflation of balloon. Ultrasound guided percutaneous puncture cannot be possible many times as there is difficulty in gaining access to balloon. Patients not presenting with ureteric injury can be managed conservatively by changing or removing the catheter. Patient with a patulous ureter did not have ureteral injury [13]. If ureteric injury is detected, Surgery should be done according to type of injury and duration until detection should be done. If detected early, then ureteric stenting should be done. If the injury is recognized late and if there are presence of complication that could be interfere with ureteral healing like abscess formation, urinary tract infection or urinary fistula formation then first proximal urinary diversion by percutaneous nephrostomy should be performed. The expected sequel of ureteric injury is ureteral stricture so long term follow up is necessary.
Reports of such cases are few and this reflects the low incidence. Male to Female ratio is 1:3. Both our patients were females. There was no difference between right and left sided ureteric involvement.
Our one patient had left, and another patient has right sided ureteric involvement. Our both patients had a history of urological disease. Both cases were diagnosed with ultrasound. One of our patients had no obvious risk factor for catheter misplacement. However, it could be done in empty bladder as it is done outside, and patient had history of oliguria. The second patient had a wide ureteric orifice so the catheter may easily pass through it. One of our patients managed non-operatively because no definite sign of ureteric injury was observed. Another patient managed operatively without ureteric stenting as no ureteric injury was found. The lack of injury might be related to patulous ureter. All previously diagnosed patients are adults as mentioned in Luo R study. Our both patients were pediatric.
Conclusion
Foley’s catheterization is a widely done invasive clinical procedure that can cause discomfort to patient. If urinary drainage following catheterization is inadequate, then the team must look for possible complications including a tip being misplaced into ureter. We do not recommend routine ultrasound imaging after catheterization. However, it is necessary when clinical suspicion arises and perform other imaging evaluations as well to look for complications related to it. Misplacement of catheter into ureter can also occur even in patients with no definite risk factors. Physicians should take care to follow the basic principles of catheterization even if the procedure is considered simple and easy to perform to avoid such complication. A multidisciplinary approach is required to manage this scenario.
References
- Ogawa K, Shimizu Y, Tsuchihashi K, Kida K, Kanamaru S, et al. (2018) Misdirection of an indwelling urethral catheter into the ureter in a female patient with neurogenic bladder: a case report. Hinyokika Kiyo 64(3): 123-126.
- Smekal M, Arumuham V, Tasleem A, Mikhail M, Allen C, et al. (2020) Retained urethral catheter in the ureter following misplaced insertion in a postpartum female. J Endourol Case Rep 6(2): 70-72.
- Cho SK, Kim MS, Chung HS, Hwang EC, Jung SI, et al. (2021) Transurethral Foley catheter misplacement into the upper urinary tract in a patient with a history of lung cancer and chemotherapy: a case report and considerations to keep in mind. Transl Androl Urol 10(3): 1347-1351.
- Qin PF, Liu WZ, Yang BB, Lu KN, Qian JH, et al. (2022) Removal of a Foley catheter misplaced into the ureter by percutaneous puncture: a rare case report. BMC Urol 22(1): 99.
- Ishikawa T, Araki M, Hirata T, Watanabe M, Ebara S, et al. (2014) A rare complication: misdirection of an indwelling urethral catheter into the ureter. Acta Med Okayama 68(1): 47-51.
- Kashefi C, Messer K, Barden R, Sexton C, Parsons JK (2008) Incidence and prevention of iatrogenic urethral injuries. J Urol 179(6): 2254-2257.
- Lowthian P (1998) The dangers of long-term catheter drainage. Br J Nurs 7(7): 366-368.
- Luo R, Lee SL, Ng FC, Koh L-T (2017) Inadvertent placement of a urinary catheter into the ureter: A report of 3 cases and review of the literature. Asian J Urol 4(4): 256-261.
- Okayama S, Matsui M, Somekawa S, Iwano M, Saito Y (2009) Non-contrast MRI for the evaluation of hydronephrotic and dysfunctioning kidney secondary to testicular cancer. Ren Fail 31(2): 153-158.
- Baker KS, Dane B, Edelstein Y, Malhotra A, Gould E (2013) Ureteral rupture from aberrant Foley catheter placement: A case report. J Radiol Case Rep 7(1): 33-40.
- McGregor TB, Sharda R (2016) Retained Urethral Catheter Secondary to Placement in Proximal Ureter. Case Rep Urol 2016: 9178645.
- Patterson R, Little B, Tolan J, Sweeney C (2006) How to manage a urinary catheter balloon that will not deflate. Int Urol Nephrol 38(1): 57-61.
- Kato H (1997) Incorrect positioning of an indwelling urethral catheter in the ureter. Int J Urol 4(4): 417-418.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





