Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1644
Research Article(ISSN: 2641-1644) 
Role of the Pharmacist in the Management of Sexually Transmitted Infections Volume 3 - Issue 1
Youness Chakir*, Yousra Merimi, Amine Moataz, Mohamed Dakir, Adil Debbagh and Rachid Aboutaieb
- Urology Department UHC Ibn Rochd, Casablanca, Morocco
Received: May 10, 2022; Published: May 19, 2022
Corresponding author: Youness Chakir, Urology Department UHC Ibn Rochd Laboratory of Sexual Health, Hassan 2 University Casablanca, Casablanca, Morocco
DOI: 10.32474/OAJRSD.2022.03.000152
Abstract
Introduction: Patients with symptomatic sexually transmitted infections initially seek health care in the pharmacy. The objectives of this work are to assess the quality and relevance of the management of sexually transmitted infections as well as to assess the knowledge, attitudes and behaviours of pharmacists.
Materials and Methods: Cross-sectional descriptive study, carried out over a period of 6 months, by means of an anonymous questionnaire, intended for community pharmacists.
Results: During the study period, 119 questionnaires were collected. The results showed that sexually transmitted infections mainly affect the young population, those aged 25-35 at 57%, with a clear predominance of the male sex at 76%. The results revealed that 72% of genital discharge, 30% of genital ulcerations and 5% of condylomas were offered treatment. It is noted that 100% of participating pharmacists ask patients questions and only 21% asked about the partner’s state of health. None of the requirements were in line with national and/or international recommendations. 52% of pharmacists have given advice on condom use and 52% offer people most at risk of HIV testing.
Conclusion: The pharmacy profession is well positioned to make a significant contribution to the prevention and control of STIs. Early detection and treatment of STIs can reduce transmission and prevent complications, and in some settings, reduce HIV transmission.
Keywords: Pharmacist; Sexually Transmitted Infections; Management; Syndromic Approach; Prevention; Screening
Introduction
Sexually transmitted infections (STIs) are a global public health problem, a priority fight for the World Health Organization (WHO). In order to better combat these STIs, WHO has proposed syndromic management. Its objective was to enable the correct diagnosis and treatment of STIs using simple algorithms at all levels of the health pyramid of countries. This strategy is adapted to the context of the scarcity of qualified human resources and the low level of the technical platform of developing countries. This syndromic management of STIs is based on the identification of coherent groups of symptoms and syndromes, and the provision of appropriate treatments to the majority of microorganisms responsible for the syndrome, or to the most dangerous of them. This is the approach that has been adopted by Morocco. Significant barriers to STI treatment include access to care and cultural and social stigma surrounding sexuality. Pharmacist-based management of STIs can provide a pathway for more accessible and timely treatment of these infections, thereby reducing the spread and long-term effects of these diseases. The main objective of this work was the evaluation of the quality and relevance of the management of sexually transmitted infections by the syndromic approach; the secondary objectives are the evaluation of the knowledge, attitudes and behaviors of pharmacists.
Materials and Methods
This is a cross-sectional descriptive study carried out by means of a questionnaire intended for pharmacists in the kingdom. Pharmacist assistants and students were excluded from this study. The questionnaire was available online from 18 July 2019 to 25 January 2020. Different parameters were explored. Concerning the pharmacist: duration of exercise in pharmacies, exercise area, knowledge on STIs, the estimate of the number of STIs received per month, the care of the pharmacist (the place of reception of the patient, the information sought, any advice provided that may be useful in the face of an STI). The profile of patients with STIs: age, sex, level of education, professional situation, medical coverage, symptoms and suspected infectious agents involved, rate of firstline use of pharmacists. All responses were subjected to descriptive statistical analysis via Excel software. The questionnaire was anonymous and the pharmacist’s consent was obtained prior to the response.
Results
One hundred and nineteen (119) responses were obtained.
The characteristics of pharmacists and patients
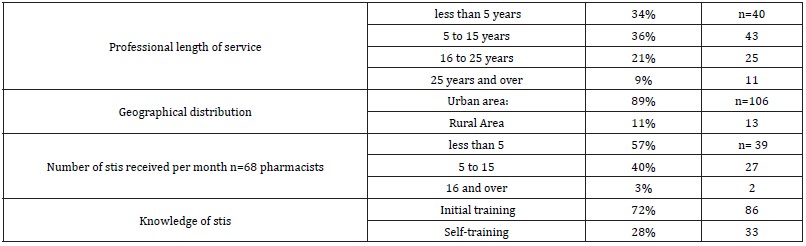
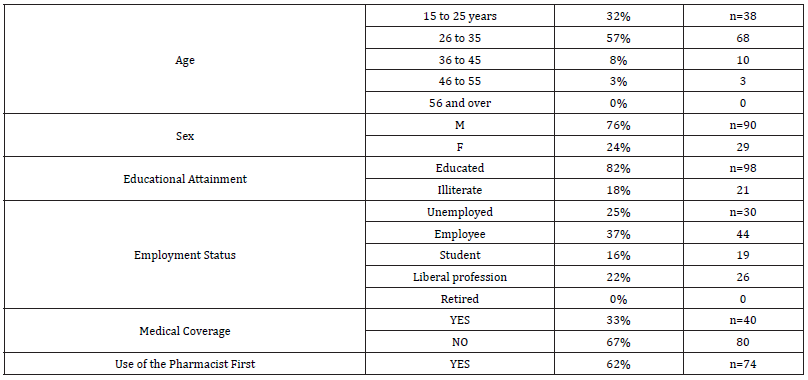
The characteristics of pharmacists are summarized in Tables 1 & 2.
Clinical manifestations of consulting patients
The clinical manifestations of STIs in men most cited by pharmacists, are respectively: urethral discharge 85%, burning urination or dysuria 73%, skin itching and pruritus 72%, swelling of the scrotum 25%, condylomas 18% and lastly swelling or inguinal ulceration 15%.
The clinical manifestations of STIs in women most cited by pharmacists are respectively: leucorrhea 91%, vulvovaginal pruritus 84%, dyspareunia 36%, pelvic pain 36%, followed by metrorrhagia 22% and condyloma 15%.
Therapeutic management of the pharmacist in front of patients with STIs
One hundred and two pharmacists (85%) received affected patients at the counter, twelve pharmacists (10%) received patients in their office and five pharmacists (4%) received patients in an area of the pharmacy that respected the patient’s privacy. The pharmacist asked about the time to onset of symptoms (72%), the symptoms of the disease (62%), the last unprotected report (60%) and subsequent drug intakes and allergies (41%). A question about reaching the partner was asked in 21% of cases. The most common STIs according to pharmacists are: Nisseria gonorrheae: 83%, genital hepes: 46%, Trichomonas vaginalis 37% as well as Treponema pallidum then Chlamydia 30% and condylomas 10%. Seventy-one percent of pharmacists delivered treatment without order, while 29% referred affected patients to a doctor.
In case of urethral discharge, fluoroquinolones including Ciprofloxacin and Ofloxacin are the most delivered antibiotics in 56%, cyclins including Doxycycline 38%, followed by Cephalosporins of 3rd generation including Ceftriaxone and Cefixime 26%, then we find antiparasitics with a percentage of 17%. Macrolides and aminoglycosides are the least recommended with a percentage of 12% and 9% respectively (Figure 1). Drugs dispensed by the pharmacist in front of vaginal discharge: Fluoroquinolones of which Ciprofloxacin and Ofloxacin are the most dispensed with a percentage of 43%, antiparasitics including Metronidazole and Tinidazole with a percentage of 40%, followed by antifungals including Econazole and Sertaconazole with a percentage of 37%, then we find Polygynaxâ Egg, with a percentage of 23%, cyclins, β-lactams and macrolides are the least recommended with a percentage of 21%, 7% and 4% respectively (Figure 2).
In the case of genital ulceration, 69% of pharmacists referred affected patients to a doctor, 3% of pharmacists dispensed medications. β-lactams including Benzathine Benzyl-Penicillin, Flucloxacillin, protected Amoxicillin and Ceftriaxone are the most delivered with a percentage of 46%, antibiotics for topical use including Fusidic Acid 27%, followed by antivirals including Aciclovir 21%, macrolides, Fluoroquinolones and cyclins are the least delivered with a percentage of 11%,8% and 3% respectively (Figure 3). In the case of genital warts: 95% of pharmacists referred patients to a doctor. Five percent advised drugs based on Imiquimod and Podophyllotoxin which is withdrawn from the market. For the pharmacist’s advice to patients are summarized in Figure 4. Regarding HIV testing of pharmacy consultants for an STI: 52% of pharmacists advise patients most at risk of HIV testing. The majority of pharmacists agreed on the point of referring any pregnant woman affected to a doctor: 88% to a specialist doctor and 10% to a general practitioner. Two percent of pharmacists recommended treatment. Finally, pharmacists in pharmacies estimate that 79% of patients are satisfied against 21% dissatisfied with the management of an STI in pharmacies.
Discussion
STIs are infections that affect a young population. In our study the most represented age group, regardless of gender, is that of patients aged 25 to 35 years (57%), followed by patients aged 15 to 25 years (3%). This age group is sexually active, has a lack of information about STIs, wants to try new experiences and has a willingness to take risks. This is consistent with the data in the literature, STIs mainly affect a young population. The World Health Organization (WHO) estimates that the prevalence and global incidence of urogenital chlamydia, gonorrhea, Trichomonas and syphilis in adult men and women aged 15 to 49 years remain high, with nearly one million new cases of curable STIs contracted every day [1]. The responsibilities of the pharmacist under Moroccan law is to prepare and deliver the drugs himself and carefully monitor the execution of all pharmaceutical acts that he does not perform himself. Every pharmacy or pharmaceutical establishment must bear the name of the pharmacist or pharmacists who own the pharmacy or products or, in the case of a pharmaceutical establishment operated by a company, the name of the pharmacists responsible or the manager. Dispensing pharmacists, distributors, wholesalers, manufacturers are required to provide all their care to the same duty: The service of the patient, by the supply, storage and dispensing of medicines of perfect quality [2].
Our study showed that 62% of patients first go to a pharmacist. Patients tend to refer to pharmacists, this can be justified by access being free and easy, the pharmacy is a natural gateway, close and available over long time slots, allowing many patients to avoid long waiting times before seeing a doctor and benefit from faster access to care. According to section 26 of this code of ethics of the pharmacist, whenever necessary, the pharmacist must encourage his clients to consult a doctor, whom he must respond with caution to requests made by patients or their attendants to know the nature of the disease treated or the value of the curative means prescribed or applied. Also, pharmacists must refrain from making a diagnosis or prognosis on the disease, in particular they must avoid commenting medically on the conclusion of the analyzes prescribed to patients [2, 3]. Our study showed a clear predominance of men with 76% compared to women 24%, i.e. a male/female ratio of 3. In our context men allow themselves far too much sexual freedom and exhibit high-risk sexual behaviour, women feel a sense of shame and fear of being misjudged, which are barriers to accessing care, so women’s low level of education, lack of awareness and information are barriers to seeking care.
In our study the main reason for consultation was urethral discharge 85%. As for women, leucorrhea 92% is the major cause of consultation. In many countries, self-medication in patients with STI syndrome and wide dispensing of drugs without a prescription by pharmacies are very common behaviors, by 31% in Thailand [4]. In Vietnam, in case of illness, 55% of people go directly to a pharmacy without going through a doctor [5]. In Switzerland, a pharmacoepidemiological survey conducted in pharmacies showed that 45% of respondents almost never consult the doctor and only 16% almost never use the pharmacist [6]. Our study found that 86% of pharmacists received STI patients over the counter. It may be because of a lack of time of the patient or pharmacist, or because the pharmacy does not have a confidentiality space, or because of fear of discrimination. The quality of the reception is a necessary condition for the patient to feel comfortable and safe, hence the need to reserve within each pharmacy a space of communication and confidentiality in order to establish a climate of trust between the patient and the pharmacist. It is the pharmacist’s role to ask the appropriate questions in order to collect the answers that will allow him to guide the diagnosis and advice. Our study showed that 100% of participating pharmacists ask questions of STI patients.
According to the code of ethics published in the official bulletin, it is stipulated that the pharmacist’s contribution to the work of health protection that the pharmacist must show the same dedication to all patients, and in order to ensure professional secrecy the pharmacist will refrain from discussing in public, especially in the pharmacy, questions relating to the diseases of his clients and their treatment [2]. The fight against sexually transmitted infections is one of the priorities of the national strategy for the prevention of HIV infection. In this context, the Ministry of Health has adopted the syndromic approach recommended by WHO for the management of sexually transmitted infections since 1998. Three algorithms have been selected for the management of urethral discharge syndromes, genital ulceration, vaginal discharge and/or lower abdominal pain. Syndromic management is simple to set up a treatment the same day, while avoiding diagnostic tests that are either expensive or essential [7,8]. According to the replies received, there is a great disparity in pharmacists’ prescriptions, in the face of genital discharge and ulceration. There is also an extremely low rate of compliance with national and/or international recommendations. This attests to a lack of knowledge of the therapeutic protocols for the management of STIs by pharmacists, this could be due to a lack of communication between pharmacists and the Ministry of Health. The pharmacist has a major role in advice and prevention, however it is important that he keep in mind that the pregnant woman requires multidisciplinary care. In some cases, the presence of an STI in a pregnant woman can influence the course of her pregnancy and imply a risk of transmission of the infection to the newborn. Education, screening, treatment and prevention are important elements of antenatal care for all women. According to our study we found that the majority of pharmacists 98% refer all pregnant women with STIs to a doctor: 88% to a specialist and 10% to a general practitioner. This testifies to a spirit of responsibility among pharmacists, that they are aware that pregnancy requires increased vigilance.
A study in more than 120 pharmacies in Birmingham, England, aimed to explore how pharmacy staffs and pharmacy users experience the provision or provision of sexual and reproductive health services. Semi-structured interviews were conducted and thematically analysed. Pharmacy users found the services convenient to use and were largely satisfied with the consultation skills of the pharmacy staffs. The Staffs were motivated to provide the services, although some felt they did not receive meaningful recognition for their work. Barriers to pharmacy sexual and reproductive health services have been identified, including lack of privacy for users, lack of trained staff, and user awareness of services. The identification of barriers to effective service delivery can be used to improve the delivery of sexual and reproductive health services in pharmacies and lead to greater care [5]. A study in Bangladesh highlights that pharmacists are well positioned to provide STI screening services, but more research is needed to overcome financial, security and privacy barriers. Short training for staff in Bangladesh’s private for-profit pharmacies helped improve their practices for advising clients with STI symptoms to use condoms and seek treatment for symptoms, as well as treatment for their partner [9]. Another study in Peru concludes that there are opportunities to train and empower pharmacists, doctors and midwives in the management of STI syndromes, thus creating a network that offers better quality in their management. The training was feasible, well accepted at Community level and appears to be effective in terms of results [10].
Another study in Peru shows that pharmacy staff who benefited from standardized simulation reported significantly better recognition and management (provision of appropriate antimicrobial diets for discharge syndromes and referral to doctors specially trained for genital ulcers or pelvic inflammatory diseases). They also reported significantly more frequent recommendations for condom use and partner treatment in pharmacies in intervention districts than in control districts. It was therefore concluded that the training was feasible and did improve pharmacists’ practices [11]. A study in England looked at the experiences of pharmacists, pharmacy health assistants and pharmacy users of a wide range of sexual and reproductive health services. The results suggest that pharmacy awareness and education was convenient to use for pharmacy users and that pharmacy staff were motivated to provide these services. However, several areas related to the nature of pharmacy, the skills of pharmacy staff have been identified where improvement could help unlock the full potential of pharmacies [12]. A literature review highlights that with training and support, pharmacy staff can serve as essential sexual health resources for youth.
More research is needed to better understand how to capitalize on the potential of pharmacy providing sexual health products to youth without sacrificing the qualities that make pharmacies so attractive to young people in the first place [13]. A systematic review concludes that users find pharmacies accessible and convenient to use, and staff find that the provision of sexual health services is feasible as part of their practice. However, barriers to service delivery include lack of privacy, limited availability of trained staff, and subjective judgments about patients [14]. A study in Ghana finds that pharmacists are well managing STIs especially urethritis. Accessibility is attractive for patients to seek STI care from pharmacists, so it is concluded that pharmacists are well positioned to provide STI screening services, but more research is needed to overcome financial, security and confidentiality barriers [15].
Conclusion
The pharmacy survey showed that most pharmacists are unaware of national and/or international STI treatment guidelines, and few pharmacists recommend HIV testing. An embarrassment, a difficulty in approaching the subject of sexuality felt by the pharmacist with the patient. The pharmacy profession is well placed to make a significant contribution to the prevention and control of STIs. Ongoing and necessary training for pharmacists for proper management of STIs.
References
- Rowley J, Vander Hoorn S, Korenromp E, Low N, Unemo M, et al. (2019) Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ 97(8): 548-562.
- Decret2-63-486 relating to the practice of the profession of pharmacist. Official bulletin of the Kingdom of Morocco.
- Dahir No. 1-06-151 of 30 Chaoual 1427 (22 November 2006) promulgating Law No. 17-04 on the Medicines and Pharmacy Code. Official Bulletin Kingdom of Morocco.
- Entz A, Prachuabmoh V, van Griensven F, Soskolne V (2001) STD history, self-treatment, and healthcare behaviours among fishermen in the Gulf of Thailand and the Andaman Sea. Sex Transm Infect 77(6): 436-440.
- Van BT, Minh KP, Strobel M (2014) Management of sexually transmitted infections in private pharmacies in Hanoi. Public Health (Bucur) 26(4): 491-498.
- Rosset C, Golay A (2006) Le pharmacien d’officine et son rôle dans l’éducation thérapeutique du patient. Rev Médicale Suisse.
- Catalogage à la source: Bibliothèque de l’OMS Le Maroc: une riposte nationale au sida. Faits marquants. (ONUSIDA collection meilleures pratiques).
- Alam N, Alam A, Fournier P (2015) Medicine Sellers for Prevention and Control of Sexually Transmitted Infections: Effect of a Quasi-Experimental Training Intervention in Bangladesh. BioMed Res Int pp: 570340.
- García PJ, Carcamo CP, Garnett GP, Campos PE, Holmes KK (2012) Improved STD Syndrome Management by a Network of Clinicians and Pharmacy Workers in Peru: The PREVEN Network. PLoS ONE 7(10): e47750.
- Garcia P, Hughes J, Carcamo C, Holmes KK (2003) Training pharmacy workers in recognition, management, and prevention of STDs: district-randomized controlled trial. Bull World Health Organ 81(11): 806-814.
- Gauly J, Ross J, Parsons J, Atherton H (2020) Staff and Users’ Experiences of Pharmacy-Based Sexual and Reproductive Health Services: A Qualitative Interview Study from the UK. Pharm 8(4): 206.
- Gonsalves L, Hindin MJ (2017) Pharmacy provision of sexual and reproductive health commodities to young people: a systematic literature review and synthesis of the evidence. Contraception 95(4): 339-363.
- Gauly J, Ross J, Hall I, Soda I, Atherton H (2019) Pharmacy-based sexual health services: a systematic review of experiences and attitudes of pharmacy users and pharmacy staff. Sex Transm Infect 95(7): 488-495.
- Mayhew S, Nzambi K, Pepin J, Adjei S (2001) Pharmacists’ role in managing sexually transmitted infections: policy issues and options for Ghana. Health Policy Plan 16(2): 152-160.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...