Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1644
Research Article(ISSN: 2641-1644) 
Impact of Varicocele Repair on the Sperm DNA Fragmentation in Infertile Men, and Reproductive Outcome Volume 3 - Issue 1
Giuseppina Peluso1 and Fabio Scarpellini2*
- 1Semen Bank and Seminology Laboratory, A.O. of Cosenza, Italy
- 2CERM Hungaria, Rome, Italy
Received: December 23, 2022; Published: NDecember 30, 2022
Corresponding author: Fabio Scarpellini, CERM Hungaria, Rome, Italy
DOI: 10.32474/OAJRSD.2022.03.000154
Abstract
Oxidative stress and related sperm DNA damage have been identified as significant causes of male infertility in men with varicocele because are usually elevated, in both abnormal and normal parameters by current World Health Organization. The current study was designed to determine to role of varicocele repair as a means of relieving SDF and improving fertility. Semen sample, from 40 patients with clinical varicocele and control group were examined. Varicocele sperm samples were classified as normal or abnormal, according to World Health Organization guidelines and Sperm DNA fragmentation evaluated pre- and post- varicocele repair. The results of study confirmed the effectiveness of varicocelectomy as a means of both reduced sperm DNA Fragmentation and improved semen quality and fertility, suggesting that varicocele repair should be offered as a part of treatment option for male partners of infertile couple.
Keywords: Varicocele treatment; male infertility; sperm DNA fragmentation; oxidative stress; varicocele repair
Introduction
Varicocele is considered one of the major causes of male infertility, found in approximately 15-20% of the general male population, a prevalence in adolescents and with frequency ranging between to 41% in men with primary infertility and 80% in those with secondary infertility. This anatomical anomaly, which appears as a dilatation of the pampiniform plexus overlying and surrounding the testicle, is probably one of the most common causes of poor sperm production and alteration of seminal parameters [1-3]. However, the pathogenetic mechanisms through which varicocele induces testicular dysfunction with consequent alteration of spermatogenesis have not yet been fully clarified [4]. Among the defects involved in this process, the most reproducible and probable would seem to be venous stasis with consequent testicular hypoxia and increase in temperature inside the testicle itself. But it is hypothesized that several factors could be involved, including oxidative stress, and it is precisely the latter that is considered one of the central pathogenetic mediators of infertility associated with varicocele [5].
Several studies in the literature on infertile patients with a clinical diagnosis of varicocele have identified oxidative stress as one of the major causes of sperm dysfunction with a negative impact on the sperm membrane, compromising its motility and ability to interact effectively with the oocyte membrane. Furthermore, it has been widely demonstrated that it alters the integrity of sperm DNA, the latter being considered fundamental in determining normal fertilization and embryonic development in spontaneous and assisted conceptions [6,7]. On the basis of these evidences, it would follow that the role of surgical correction of varicocele could be that of re-establishing a state of normal fertility by reducing the oxidative activity at the seminal level. However, this role still remains quite controversial among the various authors in the literature [8-11]. The aim of our study was to evaluate the effect of surgical correction of varicocele on semen quality and sperm DNA fragmentation in adult male subjects of infertile couples, as well as the pregnancy rate.
Materials and Methods
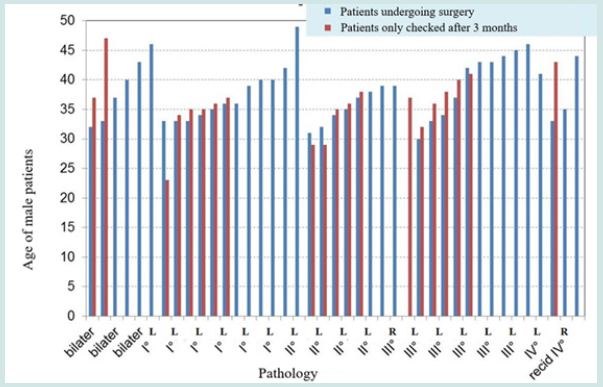
60 couples were included in the study (females aged between 25-36 years, males between 27-45 years) referred to our service for tests aimed to diagnose the causes of infertility. The male partners, investigated from an andrological point of view, presented clinical signs of varicocele, confirmed by ultrasound and scrotal color Doppler flow velocimetry ultrasound. They were also investigated from a seminological point of view with a complete examination of the seminal fluid (WHO 2010) and study of the fragmentation of sperm DNA through the use of the Halosperm test (SCD method) expressed in % DFI (DNA Fragmentation Index) [12]. In the group of patients studied, 40 of them underwent varicocele surgery, while the remaining 20 only performed controls after three months. Evaluations of seminal parameters were performed with the following criteria: 1) at the time of diagnosis of varicocele, for all patients included in the study; 2) three months after surgery for the 40 patients undergoing varicocelectomy; 3) three months after diagnosis for the 20 patients who did not undergo surgery (control group). The seminal parameters had also compared each other and correlated to the patient’s age, the degree of varicocele, the effectiveness of the intervention and controls with therapy alone (without intervention). Finally, both in the group of subjects undergoing surgery and in the control group, the spontaneous pregnancy rate or from PMA was evaluated in the 1-year follow-up.
Results
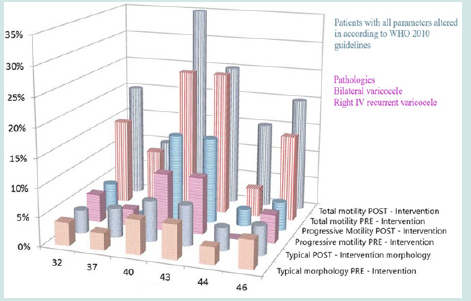
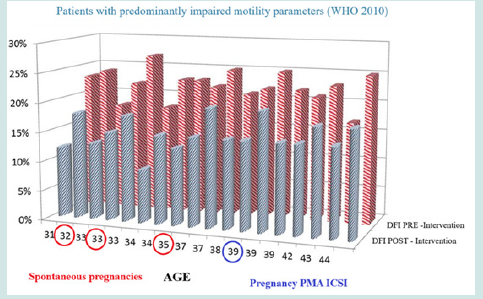
Patients with slightly altered seminal parameters benefited more from the varicocele correction surgery, restoring normal values (they returned to the WHO 2010 5th percentile) already three months after the surgery itself. The intervention led to an improvement in total motility and above all in progressive, which went from an average of 14% to an average of 20%, while remaining slightly below the parameters at the 5th percentile of the WHO 2010. The sperm DNA fragmentation index was significantly reduced for the most of the patient’s undergoing surgery, going from an average value of 27% to a post-operative average value of 19%. In the most critically ill patients (i.e., with all the seminal parameters altered), the operation was resolved only for the fragmentation of the sperm DNA (the % DFI was reduced by 15%). The patients who did not undergo surgery (control group) did not show significant changes in seminal parameters after three months and the DFI was also unchanged, passing from a value of 22% to 21%. Pregnancy rate was also observed in the one-year follow-up, in approximately 18% of patients undergoing varicocele surgery:
a) “SPONTANEOUS” in 7.5% of cases.
b) with PMA II level in 6.5% of cases.
c) with IUI in 2.5% of cases.
In the control group, spontaneous pregnancy rate was observed in the one-year follow-up, only in 5% of patients.
Data Collection
Conclusions
Our data agree with what was claimed by the various authors on the effectiveness of surgical varicocele correction in restoring natural fertility and improving outcomes in PMA [10,11-13]. Our study showed that, after the operation, there was a significant improvement in seminal parameters, especially in patients with mild forms of varicocele [13,14]. But, the most relevant data, arose from the significant reduction of sperm DNA fragmentation which occurred in all patients undergoing surgery, even the most critical ones (with severely altered semen parameters) [15-17]. Therefore, our data increasingly support the hypothesis that varicocele correction surgery may be the best semen remediation approach since it has a remarkable action in reducing sperm DNA damage and improving the fertilizing capacity of the sperm, not only in natural fertility but above all, for the purposes of PMA, where the quality of the sperm is crucial, depending fundamentally on the integrity of its DNA.
References
- Kursh ED (1987) What is the incidence of varicocele in a fertile population? Fertil Steril 48(3): 510-511.
- Molina J, Castilla JA, Castano JL, Fontes J, Mendoza N, et al. (2001) Chromatin status in human ejaculated spermatozoa from infertile patients and relationship to seminal parameters. Hum Reprod 16(3): 534-539.
- (1992) The influence of varicocele on parameters of infertility in a large group of men presenting to infertility clinic. World Health Organization. Fertil Steril 57(6): 1289-1293.
- Hauser R, Paz G, Botchan A, Yogev L, Yavetz H (2001) Varicocele and male infertility: effect on sperm function. Hum Reprod Update 7(5): 482-485.
- Pasqualotto FF, Sharma RK, Nelson DR, Thomas AJ, Agarwal A (2000) Relationship between oxidative stress, semen characteristics, and Irvine clinical diagnosis in men undergoing infertility investigation. Fertil Steril 73(3): 459-464.
- Irvine DS, Twigg JP, Gordon EL, Fulton N, Milne PA, et al. (2006) DNA integrity in human spermatozoa: relationships with semen quality. J Androl 21(1): 33-44.
- Smit M, Romijn JC, Wildhagen MF, Veldhoven JLM, Weber RFA, et al. (2010) Decreased sperm DNA fragmentation after surgical varicocelectomy is associated with increased pregnancy rate. J Urol 183(1): 270-274.
- Okeke L, Ikuerowo O, Chiekwe I, Etukakpan B,Shittu O, et al. (2007) Is varicocelectomy indicated in subfertile men with clinical varicoceles who have asthenospermia or teratospermia and normal sperm density? Int J Urol 14(8): 729-732.
- Esteves SC, Roque M, Agarwal A (2016) Outcome of assisted reproductive technology in men with treated and untreated varicocele: systematic review and meta-analysis. Asian J Androlo 18: 254-258.
- Zini A, Blumenfeld A, Libman J, Willis J (2005) Beneficial effect of microsurgical subinguinal varicocelectomy on human sperm DNA integrity. Hum Reprod 20(4): 1018-1021.
- Wang YJ, Zhang RQ, Lin YJ, Zhang RG, Zhang WL (2012) Relationship between varicocele and sperm DNA damage and the effect of varicocele repair: a meta-analysis. Reprod Biomed Online 25(3): 307-314.
- Fernàndez JL, Muriel L, Goyanes V, Segrelles E, Gosálvez J, et al. (2005) Simple determination of sperm DNA fragmentation with an improved sperm chromatin dispersion (SCD) test. Fertil Steril 84(4): 833-842.
- Esteves SC, Chan P (2015) A systematic review of clinical practice guidelines and best practice statements for the evaluation of the infertile male. Int Urol Nephrol 47(9): 1441-1456.
- Tisco BC, Esteves SC, Cocuzza MS (2016) Summary evidence on the effects of varicocele treatment to improve natural fertility in subfertile men. Asian J Androl 18: 239-245.
- Esteves SC, Santi D, Simoni M (2020) An update on clinical and surgical interventions to reduce sperm DNA fragmentation in infertile men. Andrology 8(1): 53-81.
- Qiu D, Shi Q, Pan L (2021) Efficacy of varicocelectomy for sperm DNA integrity improvement: a meta-analysis. Andrologia 53(1): e13885.
- Wang SL, Bedrick BS, Kohn TP (2021) What is the role of varicocelectomy in infertile men with clinical varicoceles and elevated sperm Dna fragmentation? Fertil Steril 116(3): 657-658.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...