Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Review Article(ISSN: 2637-4544) 
Trends and Factors Associated with Maternal Mortality at the Pre-COVID-19 era: A Retrospective Cross-Sectional Study in a University Teaching Hospital in Nnewi, Nigeria Volume 5 - Issue 2
Charlotte B Oguejiofor1,2, James E Okonkwo2, John E James2, George U Eleje1,2*, Obinna C Okafor2, Chukwuemeka COkoro2, Chigozie G Okafor2, Chijioke O Ezeigwe1,2, Michel C Egbuniwe3, Boniface U Odugu4, Sylvester O Nweze4, Ekene A Emeka5, Chika I Ofiaeli5, Nnanyereugo L Onah4, Ifeanyi J Onyekpa4, JohnBosco E Mamah6, Uchenna C Chijioke-Ofoma7, Chinekwu Sochukwu Anyaoku5, Theophilus N Agbo2, Obiora Donatus Ugwu2, Onyeka C Ekwebene8
- 1Department of Obstetrics and Gynaecology, Nnamdi Azikiwe University, Awka, Nigeria
- 2Department of Obstetrics and Gynaecology, Nnamdi Azikiwe University Teaching Hospital, Nnewi, Anambra State, Nigeria
- 3Faculty of Health Sciences & Wellbeing, University of Sunderland, United Kingdom
- 4Department of Obstetrics and Gynecology, ESUT Teaching Hospital, Parklane, Enugu, Nigeria
- 5Department of Family Medicine, Nnamdi Azikiwe University Teaching Hospital, Nnewi, South-east, Nigeria
- 6Department of Obstetrics and Gynecology, Alex Ekwueme Federal University Teaching Hospital, Abakaliki, Nigeria
- 7Department of Public Health, North Dakota State University, Fargo, United States
- 8Department of Biostatistics and Epidemiology, East Tennessee State University, Johnson City, Tennessee, United States
Received:June 28, 2023;Published:July 03, 2023
Corresponding author:George U Eleje, Department of Obstetrics and Gynaecology, Nnamdi Azikiwe University, Awka, Nigeria
DOI: 10.32474/IGWHC.2023.05.000223
Abstract
Background:Compared to industrialized nations where maternal health indicators are good, the maternal mortality rate is still high in low- and middle-income countries. Due to their importance in helping Nigeria and other low- and middle-income nations plan better maternity care delivery, factors that contribute to it could be addressed through routine audits and inquiries.
Objectives:To determine the causes and features of maternal deaths, the present maternal mortality ratio, and the evolution of maternal mortality over the research period
Methods: The study is a retrospective analysis of all maternal deaths that occurred between January 1, 2013, and December 31, 2017, at Nnamdi Azikiwe University Teaching Hospital (NAUTH), Nnewi, Nigeria. Maternal mortality ratio, risk variables, and causes of maternal death were the outcome measures. Data were gathered from the prenatal, maternity, labour, and delivery wards as well as the medical records department. The statistical analysis was conducted using the statistical package for social sciences (SPSS) version 26.0.
Results: Over the course of the study’s five years, a total of 6,930 deliveries were documented. Of those, 92 maternal deaths were also reported, amounting to a maternal mortality ratio (MMR) of 1328 per 100,000 live births. Patients with and without appointments were included in the study. Of all the maternal dealths, 88 were unbooked and this constitutes 95.8% of all maternal deaths. The study found that most of the scheduled patients who had maternal deaths were those who were irregular with their prenatal appointments and prescriptions, which prevented early detection of their disorders. The main causes of these deaths were poverty, primigravidity, primparity, grandmultiparity, delivery from traditional delivery attendants, maternity homes, and substandard private hospitals. Urban residents were responsible for 62% of parturient deaths compared to rural residents, which was explained by the concentration of poor-quality private hospitals and maternity homes in urban areas. Petty traders and unskilled labourers also had high rates of maternal mortality, demonstrating the importance of poverty in the cause of maternal mortality. Preeclampsia/eclampsia (24.2%), obstetric haemorrhage-antepartum and postpartum (23.1%), puerperal infection (13.3%), and uterine rupture (21.3%) were the most frequent causes of maternal death throughout the study period.
Conclusion: The hospital has high MMR indices. High rates of maternal death in Nigeria have consistently been an embarrassment to the obstetrics profession. This is due to the ongoing inability to put into practice the safe motherhood initiatives tried-andtrue strategies, which will guarantee the delivery of emergency obstetric care and the accomplishment of the global millennium developmental goals with regard to maternal health.
Key words:Maternal Mortality; Maternal Death; NAUTH; Nnewi
Introduction
No matter the length or location of the pregnancy, maternal mortality is defined as the death of a woman while she is pregnant or within 42 days of the pregnancy’s termination from any cause associated with or aggravated by the pregnancy itself or its management, but not from accidental or incidental causes [1- 3]. Pregnancy is a journey filled with high hopes. The expectant mother, her close family, and friends eagerly anticipate the birth of a new kid, and when this does not occur, the people feel bad. Maternal mortality is uncommon in rich nations where there are sufficient people and material resources to save a pregnant woman. In contrast, pregnancy is still seen as a dangerous journey in low- and middle-income nations where unnecessary fatalities still happen. The effects of maternal death extend well beyond the immediate family and community. One of society’s most devastating catastrophes has occurred. Obstetrics practice in underdeveloped nations continues to be tainted by the tragedy of maternal mortality [2]. Maternal mortality rates are higher in underdeveloped nations than in developed ones, according to health statistics compiled by the World Health Organization, WHO, where the latter was determined to have contributed only 1% to maternal mortality. Contrarily, low and middle-income-country women of reproductive age, who make up 75% of all women of reproductive age globally, also account for 99% of all maternal deaths3. The Safe Motherhood Initiatives, which were introduced in Kenya in 1987, as well as the Millennium Development Goals (MDGs) and Sustainable Development Goals (SDGs) of the United Nations (2000 and 2015, respectively), were all intended to reduce maternal mortality. Despite their introduction, however, maternal deaths have persisted in alarming numbers, particularly in Sub-Saharan Africa (SSA) [4,5]. According to research, the probability of a woman dying during pregnancy is 1 in 13 in Sub-Saharan Africa, compared to 1 in 4055 in some wealthy nations [2]. Measures to lower maternal mortality include those that are part of the Millennium Development Goals 3, and 5. It holds that if the lofty goals of the Safe Motherhood Initiative and the Millennium Development Goals are implemented, there will be a significant decrease in maternal deaths, but the situation has not changed because maternal deaths have continued to rise in Sub-Saharan Africa and other parts of the world [5]. In reality, due to the fact that some maternal deaths in developing nations go unreported or are underreported, maternal mortality has been called a myriad of quiet tragedies [6]. The World Health Organization estimates that 830 women die each day from pregnancy- and childbirth-related avoidable causes [7]. Nigeria, although having less than 1% of the world’s population, has a disproportionately high maternal mortality rate. Nigeria was responsible for 1 in 5 and 1 in 4 of all maternal deaths worldwide and in the region, respectively, in 2015 [8]. In reality, 135 Nigerian women lose their lives during childbirth every day; if nothing drastic is done, one will die every 10 minutes [9]. The majority of maternal death rates reported in Nigeria are based on hospital data, and they range from 460 to 2200, with an average of 1100 per 100,000 live births. The high prevalence of gender inequality and the under-empowerment of women of reproductive age in Nigeria, as in the majority of low and middle-income countries, have been cited as the causes of maternal mortality [10,11]. It is allegedly a problem that is not well acknowledged. In light of the foregoing, obstetricians must continually assess their efforts to combat the epidemic of maternal mortality, determine whether those efforts have been fruitful, and remind themselves of the importance of bringing this tragedy to the forefront of public discourse in order to draw attention to the tragedy’s neglect. Therefore, the purpose of this study is to ascertain the Maternal Mortality Ratio (MMR), the reasons for maternal deaths, their trends, and their features in NAUTH, Nnewi.
Materials and Methods
Study Design and Setting
All maternal deaths that happened at NAUTH over a fiveyear period, from January 1, 2013, to December 31, 2017, were the subject of this retrospective analysis. The teaching hospital of Nnamdi Azikiwe University is situated in Nnewi. One of the commercial hubs of the state of Anambra is Nnewi town. The Chukwuemeka Odomegwu Ojukwu University Teaching Hospital (COOUTH), Awka, is the other of the two referral tertiary facilities in Anambra state. Offering undergraduate and graduate study in a variety of medical specialties, including obstetrics and gynaecology, is the Nnamdi Azikiwe University Teaching Hospital. It acts as a referral hospital for the region’s states, including Delta, Imo, Enugu, and Abia.
Study Population and Data Collection
Data were gathered from the registers of all hospital departments that cared for expectant mothers, including the intensive care units, labour ward, theater, ante-natal, postnatal, and gynecology ward. The information on every patient who received care throughout the review period was carefully retrieved from their case records. The data taken from this record comprised the number of maternal deaths, the booking status, the patient’s age, parity, marital status, occupation, educational attainment, the length of hospital stay before to death, the referral centers, and the causes of death.
Outcome Measures
The outcome measures were maternal mortality ratio, risk factors and causes of maternal mortality.
Study Analysis
The data collected were analyzed using Statistical Package for Social Sciences (SPSS) version 26.0. The results were represented in a simple frequency table and percentages.
Ethics Approval
The present study was approved by the hospital’s ethics Committee (No. 0156/10/2022).
Results
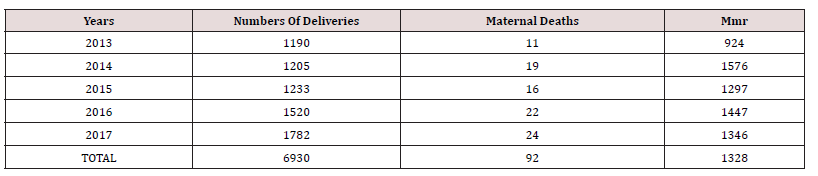
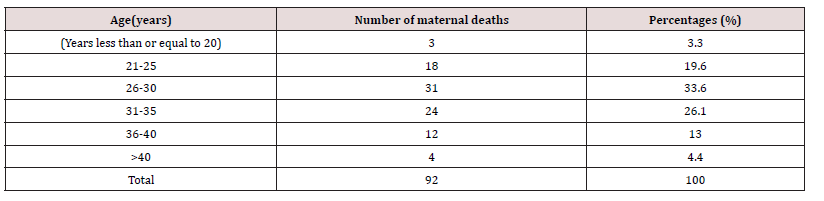
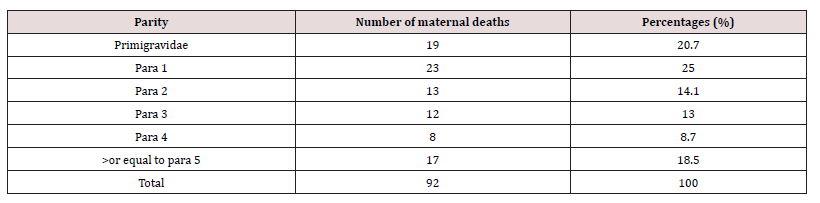
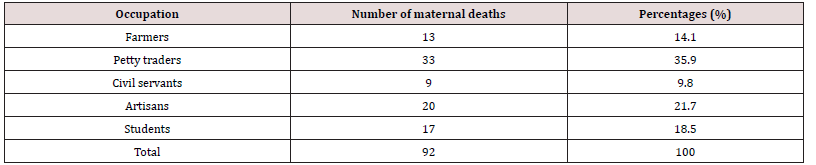
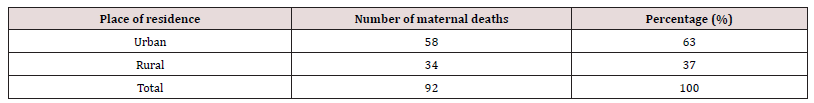
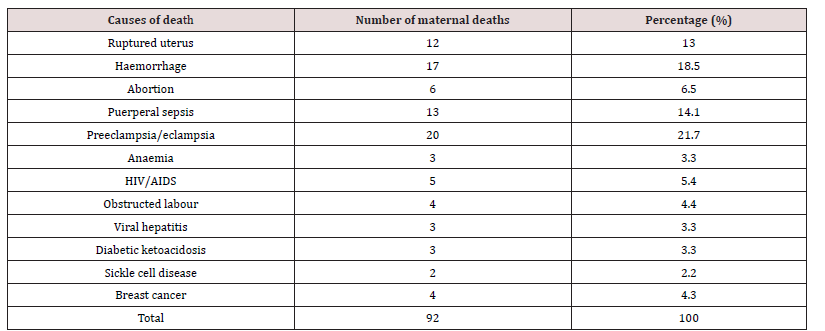
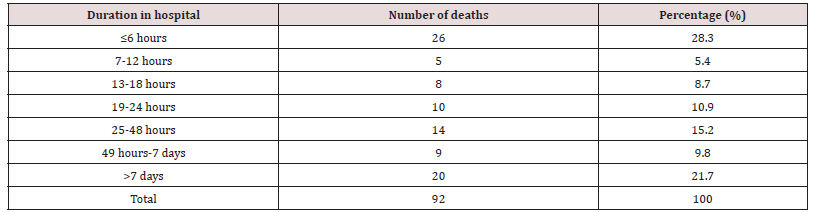
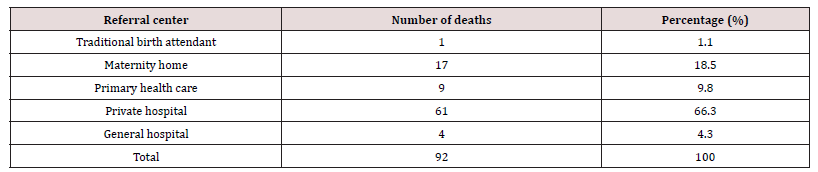
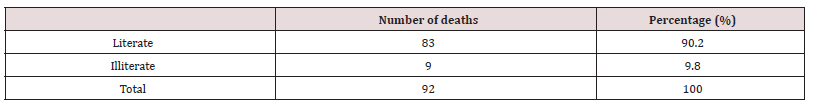
There were 6930 live births registered overall throughout the study period between 1 January 2013 and 31 December 2017, and 92 maternal deaths were also noted. 1328 deaths due to maternal causes were recorded for every 100,000 live births. Maternal mortality varies between 924 per 100,000 and 1576 per 100,000 live births, according to annual analyses. Table 1 shows the actual Maternal Mortality Ratio (MMR). It demonstrates that the lowest maternal mortality ratio (924 per 100,000 live births) and highest MMR (1576 per 100,000 live deliveries), respectively, were recorded in 2013 and 2014. The age distribution of maternal fatalities throughout the time period under consideration is analyzed in Table 2. Women between the ages of 26 and 30 had the highest percentage (33.6%). The lowest rate of maternal deaths- 3.3%-occurred in the age group under 20. Table 3 shows the effect of parity on maternal mortality. Women who are para 1 had the highest maternal mortality of 25.0% compared to women of other parities. Table 4 demonstrated that, when compared to women who died from other professions, small traders had the greatest maternal mortality rate, reaching up to 35.9% during the time. According to the survey, civil servants experienced the fewest fatalities. Table 5 displays the impact of residency on maternal fatalities and makes it abundantly evident that urban inhabitants died more frequently than rural ones. Preeclampsia and eclampsia were the primary causes of maternal death, and obstetric haemorrhage was the second-most common cause, according to Table 6. Unsafe abortion, uterine rupture, sepsis, diabetic keto-acidosis, anaemia, viral hepatitis, HIV/AIDS, and liver and breast malignancies were other causes.
MMR: maternal mortality ratio per 100,000 live births.
Discussions
The maternal mortality ratio varies from location to location,
hospital to hospital, and even over time within a single hospital.
In Nigeria and other nations, particularly in sub-Saharan Africa,
maternal death is a tragedy that is getting worse but is preventable.
Maternal mortalities are typically evaluated sporadically in the
obstetric department to see whether such deaths were avoidable.
With adequate auditing, there is typically improvement with
interventions as a result of this persistent problem in obstetric
practice in impoverished nations. During the five-year period,
there were 1328 maternal deaths for every 100,000 live births. The
study’s maternal mortality rate of 1328 per 100,000 live births is
higher than the rates found in some other low - and middle-income
nations, including Tanzania 556 [12], Uganda 31[13], Zimbabwe
217 [14], Egypt 89 [15], Ethiopia 590 [16], and other states in
Nigeria, including 1098 in Nnewi [6] and 518 in Benin City [17].
This maternal mortality ratio was within the range of the country’s
maternal mortality ratio, which ranges from 460 to 2,200 with an
average of 1,100 [18]. It was somewhat higher than the national
average of 814 per 100,000 live births. These variations could be
caused by the varying sociodemographic characteristics of the
expectant mothers as well as the accessibility, use, and acceptance
of emergency obstetrics services by the various populations
under study. The variations could also be a result of the various
populations being investigated. In addition, it was determined that
attendant delays at home before hospital presentation, poverty,
ignorance, and subpar care offered in maternity homes and private
hospitals were to blame for the unacceptable high maternal
mortality percentages (Tables 7-9).
The majority of women who had maternal mortality in the study hospital were young, with those between the ages of 21 and 35 accounting for 82.2%. When women do not receive adequate antenatal care, maternal mortality often occurs during their most productive and prime years of life. This was in line with the findings of Igwegbe et al., who stated that postpartum mortality affected the majority of women (79.2%) [6] who were in the 31-35 age range, had 0–1 children (58.4%), and were “unbooked” (85.4%). This is reportedly because they arrived in lifeless conditions after trying unconventional remedies for the treatment of severe labour problems. In low- and middle-income nations, it can be difficult and stressful to provide emergency obstetric treatment for unbooked patients because most of the women who arrive at the hospital are unable to pay for the necessary supplies. These unbooked ladies represent a high-risk population, according to this. Due to their poor socioeconomic status, petty traders accounted for 35.9% of all maternal fatalities. According to the survey, a higher percentage of urban residents died than those who lived in rural areas. Preeclampsia/eclampsia is the largest cause of maternal mortality worldwide, and the same factor was seen in this study [6]. Preeclampsia and eclampsia are widespread in our society, reportedly as a result of several unqualified, substandard maternity homes and certain private hospitals where these women receive antenatal care but are not adequately examined for preeclampsia or eclampsia. Obstetric haemorrhage, whether antepartum or postpartum, is the second most common cause of death in this study. Obstetric haemorrhage is made worse by the societal stigma attached to voluntary blood donation. The third most frequent cause of maternal death in the study was puerperal sepsis. This might be related to antibiotic misuse, poor quality antibiotic use, and careless antibiotic use in our environment.
The fourth cause of maternal mortality in this study, ruptured uterus, was possibly caused by the maternity homes’ and some private hospitals’ inappropriate administration of oxytocin, even in women who had previously had caesarean sections. Some of the study’s findings were consistent with research carried out at various points in time in the same tertiary hospital. For instance, research conducted by Igwegbe et al at the study center in 2012 found that sepsis (8.3%) and haemorrhage (18.8%) were the two most prevalent direct causes of maternal mortality, respectively, and that pre-eclampsia/eclampsia was the most common indirect cause of maternal death (25.0%) [6]. Similar to this, research conducted by Obiechina et al. on the contribution of indirect obstetric death to maternal mortality in NAUTH, Nnewi revealed that the increase in maternal mortality is caused by numerous subpar maternity homes and private hospitals where patients are mismanaged before they present to teaching hospitals. Emergency obstetric treatment and the presence of trained delivery attendants could avert some maternal deaths. The quality of care provided in private hospitals and the successful training of the midwives who manage these maternity homes should be reviewed, with a focus on early detection of high-risk cases and an efficient referral network to secondary and tertiary clinics. Additionally, municipal and state governments should set up community-based ambulances, health posts, and comprehensive health care facilities linked to wellequipped tertiary clinics for simple referrals. The following are the limitations of our investigation. First, it was a retrospective study with unavoidable inherent biases. Second, we were unable to ascertain whether there were variations between the pre-COVID and intra-COVID periods. Future research is necessary in light of the availability of clinical data. Additionally, this study failed to distinguish between the pre- and post-COVID-19 eras. To quantify such study gaps, a well-powered retrospective cohort study is required.
Conclusion
The hospital has high MMR indices. Maternal mortality is a complicated problem with multiple causes and multiple potential remedies. Everyone has a responsibility to implement efforts to reduce maternal mortality. This study suggests that if all hands are on deck, maternal mortality could be avoided or at the very least decreased. Obstetricians must be on standby to combat this under recognized tragedy, especially when the women are admitted to hospitals, in order to lessen its epidemic. It is necessary to monitor the operators of maternity homes. The construction of a referral network and the retraining of midwives will be beneficial. Obstetricians need to make an effort to get the attention of decisionmakers. Maternal mortality will be reduced, and maternal health requirements will be better met with ongoing evaluation of efforts and results. To reverse this awful trend, poverty, ignorance, and illiteracy must be eradicated. Infrastructure needs to be developed, and women’s empowerment must become a reality.
Acknowledgements
The authors would like to thank the Medical Record Department, Resident doctors, and nurses for releasing the data utilized in the study.
Author Contributions
All the authors were involved in the overall conceptual design and implementation of the project, and overall revision of the manuscript. CBO, OCO, CGO, JEO, JEJ, TNA, ODU and COE contributed to data collection, analysis, and manuscript writing. BUO, GUE, SON, EAE, CCO, CIO, IJO, MCE, JEM, UCC, CSA, OCE and NLO were involved in the writing of this manuscript and overall revision. The authors read, approved the final manuscript, and agreed to be accountable for all aspects of the work.
Disclosure Statement for Publication
All authors have made substantial contributions to conception and design of the study, or acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version submitted. This manuscript has not been submitted for publication in another journal.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval and Consent to Participate
The study was approved by the Ethics Review Board of the hospital (Reference number: 0156/10/2022; date of approval: 26th October 2022)..
References
- Oyeneyin L, Akintan A, Aderoba A, et al. (2017) Maternal mortality ratio in a tertiary hospital offering free maternity services in South-western Nigeria -A five-year review. Trop J Obstet Gynaecol 34: 112.
- Ibong Akpanekpo E, David Umoessien E, Ime Frank E (2017) Unsafe Abortion and Maternal Mortality in Nigeria: A Review. Pan African Journal of Medicine.
- Goli S, Puri P, Salve PS, Saseendran Pallikadavath, James KS (2022) Estimates and correlates of district-level maternal mortality ratio in India. PLOS Glob Public Heal 2(7): e0000441.
- Azuh DE, Azuh AE, Iweala EJ, Davies Adeloye, Moses Akanbi (2017) Factors influencing maternal mortality among rural communities in southwestern Nigeria. Int J Womens Health 9: 179-188.
- Ronsmans C, Graham WJ (2006) Maternal mortality: who, when, where, and why. Lancet 368 (9542): 1189-1200.
- Igwegbe AO, Eleje GU, Ugboaja JO, Ofiaeli RO (2012) Improving maternal mortality at a university teaching hospital in Nnewi, Nigeria. Int J Gynaecol Obstet 116(3): 197-200.
- Olonade O, Olawande TI, Alabi OJ, David Imhonopi (2019) Maternal mortality and maternal health care in Nigeria: Implications for socio-economic development. Open Access Maced J Med Sci 7(5): 849-855.
- Ariyo O, Ozodiegwu ID, Doctor H V (2017) The influence of the social and cultural environment on maternal mortality in Nigeria: Evidence from the 2013 demographic and health survey. PLoS ONE 12(12): e0190285.
- Piane GM (2019) Maternal Mortality in Nigeria: A Literature Review. World Med Heal Policy 11(1): 83-94.
- Meh C, Thind A, Ryan B, Amanda Terry (2019) Levels and determinants of maternal mortality in northern and southern Nigeria. BMC Pregnancy Childbirth.
- Matthew O, Adeniji A, Osabohien R, Olawande Tomike, Tolulope Atolagbe (2020) Gender Inequality, Maternal Mortality and Inclusive Growth in Nigeria. Soc Indic Res 147(2): 763-780.
- Bwana VM, Id SFR, Mremi IR, Emanuel P Lyimo, Leonard EG Mboera (2019) Patterns and causes of hospital maternal mortality in. PLoS One 24: 1-22.
- Serbanescu F, Goldberg HI, Danel I, Tadesse Wuhib, Lawrence Marum, et al. (2017) Rapid reduction of maternal mortality in Uganda and Zambia through the saving mothers, giving life initiative: Results of year 1 evaluation. BMC Pregnancy Childbirth 17(1): 1-14.
- Musarandega R, Cresswell J, Magwali T, Davidzoyashe Makosa, Rhoderick Machekano, et al. (2022) Maternal mortality decline in Zimbabwe, 2007/2008 to 2018/2019: findings from mortality surveys using civil registration, vital statistics and health system data. BMJ Glob Heal 7(8): 1-11.
- Abbas A, Amin M, Ali S, Neima Z Salem (2016) Maternal mortality: a tertiary care hospital experience in Upper Egypt. Int J Reprod Contraception Obstet Gynecol 5(5): 1466-1471.
- Berhan Y, Berhan A (2014) Review of maternal mortality in Ethiopia: a story of the past 30 years. Ethiop J Health Sci 24: 3-14.
- Abe E, Omo Aghoja LO (2008) Maternal mortality at the Central Hospital, Benin City Nigeria: a ten year review. Afr J Reprod Health 12(3): 17-26.
- Mbachu II, Ezeama C, Osuagwu K, Osita Samuel Umeononihu, Chibuzor Obiannika, et al. (2017) A cross sectional study of maternal near miss and mortality at a rural tertiary centre in southern nigeria. BMC Pregnancy Childbirth 17(1): 251.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...