Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Review Article(ISSN: 2637-4544) 
Prevalence and Predictive Factors of Female Sexual Dysfunction in Saudi Arabia: A Cross-sectional Study Volume 5 - Issue 2
Maysoon Alhaizan1*, Ghadah Algudairi2, Dana Aldabeeb1, Maha Alhainiah1, Rahaf Alharthy1, Saleh Binsaleh3, Ghadeer Alshaikh1
- 1Department of Obstetrics & Gynecology, King Saud University, Riyadh, Saudi Arabia
- *Physical Therapy Department, Security Forces Hospital, Riyadh, Saudi Arabia
- 2Urology Unit, Department of Surgery, King Saud University, Riyadh, Saudi Arabia
Received:August 09, 2023;Published:August 17, 2023
Corresponding author:Maysoon Alhaizan, Department of Obstetrics & Gynecology, King Saud University, Riyadh, Saudi Arabia
DOI: 10.32474/IGWHC.2023.05.000225
Abstract
Introduction: Female Sexual Dysfunction (FSD) adversely affects multiple aspects including quality of life, interpersonal
relationships, and self-esteem. It takes different forms, including lack of sexual desire, impaired arousal, inability to achieve
orgasm, and pain with sexual activity. It is reported in approximately 30-60% of females worldwide. FSD has not been adequately
investigated in Saudi Arabia for several reasons.
Aim: To assess the prevalence and predictors of FSD in a community-based sample of Saudi women.
Method: This cross-sectional study included a convenience sample of Saudi women aged 20 years or older who were sexually
active. Data were collected using a validated questionnaire consisting of multiple variables, including female demographic data and
the Female Sexual Function Index [FSFI]. The Validated Arabic version of the FSFI [ArFSFI] was used to assess FSD.
Results: A total of 822 participants were included and a total of 459 (55.8%) had FSD (FSFI ≤26.55). FSD was positively
associated with taking medications, especially antidepressants (p<0.001), longer duration of marriage (p<0.001), higher number
of deliveries (p<0.001), menopause (p=0.001), need for lubricants (p<0.001), encountering sexual assault (p=0.042), and lower
ratings of relationships with partners (p<0.001). The domain with the lowest score was desire (3.47±1.22), followed by arousal
(3.76±1.48), orgasm (4.04±1.61), pain (4.24±1.54), satisfaction (4.24±1.60), and lubrication (4.35±1.39).
Conclusion: The estimated prevalence of FSD in Saudi women is 56%. Desire and arousal were the most significantly affected
domains, followed by orgasmic problems. The most important risk factor for FSD is antidepressant use. More studies that implement
structured interviews with both partners to examine risk factors and predictors are strongly warranted. Finally, it is essential to
educate women about the types of FDS and overcome cultural barriers to provide a better quality of life.
Keywords: Female Sexual Dysfunction; Female Sexual Function Index; Saudi; Prevalence; Risk Factors.
Plain Language Summary
Female Sexual Dysfunction (FSD) adversely affects multiple
aspects including quality of life, interpersonal relationships,
and self-esteem. It takes different forms, including lack of sexual
desire, impaired arousal, inability to achieve orgasm, and pain with
sexual activity. It is reported in approximately 30-60% of females
worldwide. FSD has not been adequately investigated in Saudi
Arabia for several reasons. Our aim is to assess the prevalence and
predictors of FSD in a community-based sample of Saudi women.
This study included a convenient sample of Saudi women aged 20
years or older who were sexually active. We used a questionnaire
consisting of multiple variables, including female demographic data
and an index that measures Female Sexual Function [FSFI]. A total
of 822 females were included and a total of 459 (55.8%) had FSD.
FSD was positively associated with taking medications, especially
antidepressants, longer duration of the marriage, a higher number
of deliveries, menopause, need for lubricants, encountering sexual
assault, and lower ratings of relationships with partners. Desire
and arousal were the most significantly affected domains, followed
by orgasmic problems. The most important risk factor for FSD
is antidepressant use. More studies that implement structured
interviews with both partners to examine risk factors and
predictors are strongly warranted. Finally, it is essential to educate
women about the types of FDS and overcome cultural barriers to
provide better quality of life.
Introduction
Sexual function is a fundamental component of life, and dysfunction can negatively affect an individual’s well-being [1]. Female Sexual Dysfunction (FSD) is a sexual problem associated with anatomical, physiological, medical, psychological, and social components that adversely affect multiple aspects of an individual’s life, including the quality of life, interpersonal relationships, and self-esteem[2]. FSD takes different forms, including a lack of sexual desire, impaired arousal, and inability to achieve orgasm or pain with sexual activity. Although each condition can be defined separately in medical terms, there is significant clinical overlap in the affected patients [1,3]. According to the Diagnostic and Statistical Manual of Mental Diseases, sexual dysfunction is a disturbance in the sexual response cycle or pain associated with sexual intercourse[4] and it is reported in approximately 30-60 percent of women worldwide [1,5]. FSD in Saudi Arabia was reported by Madbouly et al. in their study using a clinic-based survey involving 200 Saudi women attending primary care and gynecology clinics at a University Hospital in Riyadh. They reported that (88.5%) were relatively satisfied or satisfied with their partner’s sexual ability and 120 (60%) had a risk of FSD [5]. The prevalence of FSD varies worldwide as it is caused by multiple factors and can be associated with age, socioeconomic status, degree of education, employment, biological, medical, and psychological factors [3,6]. Although FSD is highly prevalent, it remains an underestimated health problem[3,7]. Female sexual function and FSD can be evaluated in multiple ways, including by questionnaires, structured interviews, or taking a thorough case history. Questionnaires are initially used to screen individuals into different FSD categories [1,5]. The Female Sexual Function Index (FSFI) is a validated 19-item multidimensional self-report measure that quantifies six domains, including desire, arousal, lubrication, orgasm, satisfaction, and pain, for evaluation of sexual function in women [8]. The FSFI has been used to determine sexual dysfunction among female populations in various countries [1,3,7], and the Arabic Version of the Female Sexual Function Index (ArFSFI) has been validated and regarded as a reliable tool for FSD assessment in the Arabic world [9]. FSD has been inadequately investigated in Saudi Arabia for many reasons; this can be mainly attributed to women’s hesitancy to discuss their sexuality and sexual health. Moreover, published reports on the prevalence and risk of FSD in Saudi Arabia are scarce. Therefore, in this study, we aimed to assess the prevalence and predictors of FSD in a large community-based sample of Saudi women. Overall, gaining knowledge about FSD and its risk factors may have public health and clinical implications, and understanding its nature and prevalence might help to increase awareness, improve treatment, and decrease the probability of adverse outcomes.
Methods
In this cross-sectional study, we administered a communitybased questionnaire to Saudi women from November 2022 to February 2023. The questionnaires were disseminated online through social media platforms, such as Twitter and WhatsApp. Inclusion criteria were as follows: non-pregnant, non-lactating Saudi women aged 20 years and older, sexually active during the past 6 months, able to give consent, and able to understand and read Arabic. Participants with missing data were excluded from this study.
Questionnaire
Data were collected using online questionnaires. The participants spent approximately five minutes answering the questionnaire. The questionnaire consisted of multiple variables, including female demographic data such as age, marital status, number of pregnancies, education, income, and employment status. Data on working hours, work environment, chronic medical conditions, and medication use were collected. The FSFI was used to assess sexual function or problems that had occurred during the past four weeks. According to the FSFI, sexual function domains include sexual desire, arousal, lubrication, orgasm, satisfaction, and pain during sexual intercourse. Sexual desire was assessed in terms of the frequency and desire level by asking two questions. Arousal was assessed in terms of frequency, level, confidence, and satisfaction by asking four questions. Lubrication was assessed in terms of frequency, difficulty, frequency of maintaining lubrication, and difficulty in maintaining lubrication by asking four questions. Orgasm was assessed in terms of frequency, difficulty, and satisfaction by asking three questions. Satisfaction was assessed as the amount of partner closeness, sexual relationships, and overall sex life by asking three questions. Pain was assessed as pain frequency during vaginal penetration and pain frequency following vaginal penetration using three questions. The FSFI has been used to determine sexual dysfunction in female populations in different countries. The Arabic version of the FSFI was adapted and translated from its English version, while retaining the same format as the original FSFI [9]. The ArFSFI total score and scores of various domains showed high test-retest reliability (r = 0.92 to 0.98) and the ArFSFI domains showed high internal consistency (r = 0.85 to 0.94).
Ethical Approval
All procedures were consistent with the ethical standards of the Institutional Research Committee. The study was approved by Institutional Review Board [IRB] at King Saud University Medical City [KSUMC] (reference number: 18/0279/IRB) in February 2021. The purpose and aim of the study were explained at the beginning of the questionnaire to all recruited subjects and an informed written consent form was obtained from all the participants before starting the questionnaire. Participation was voluntary, and complete privacy was ensured.
Statistical Analysis
Categorical data are presented as frequencies and percentages, while continuous data are presented as mean and standard deviation (SD). The overall and domain specific FSFI scores were calculated by summing the relevant responses. In addition, the points were transformed into a 100-scale to facilitate interpretation. FSD was defined as an FSFI score ≤26.55. Demographic characteristics as well as the medical, marital, and sexual histories of the participants were compared according to the FSD status. The Chi-square or Fisher’s exact test, as appropriate, was used to examine differences in categorical variables, while the student’s t-test or Mann Whitney U test, as appropriate, was used to examine differences in continuous variables. A multivariate logistic regression analysis model was run to detect factors independently associated with FSD, after adjusting for the variables that were significantly associated with FSD in the univariate analysis (Tables 1 & 2). Backward elimination was used to allow non-significant variables to leave the model. All P-values were two-tailed and statistical significance was set at p < 0.05. Unless otherwise mentioned, SPSS (version 25.0. Armonk, NY: IBM Corp) was used for all statistical analyses.
Results
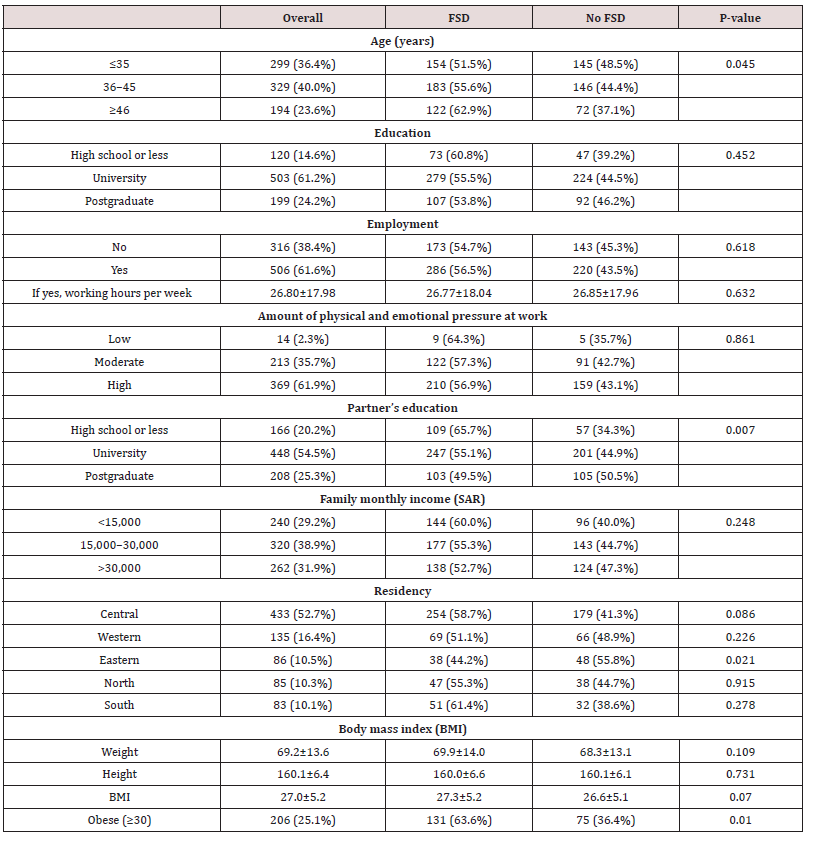
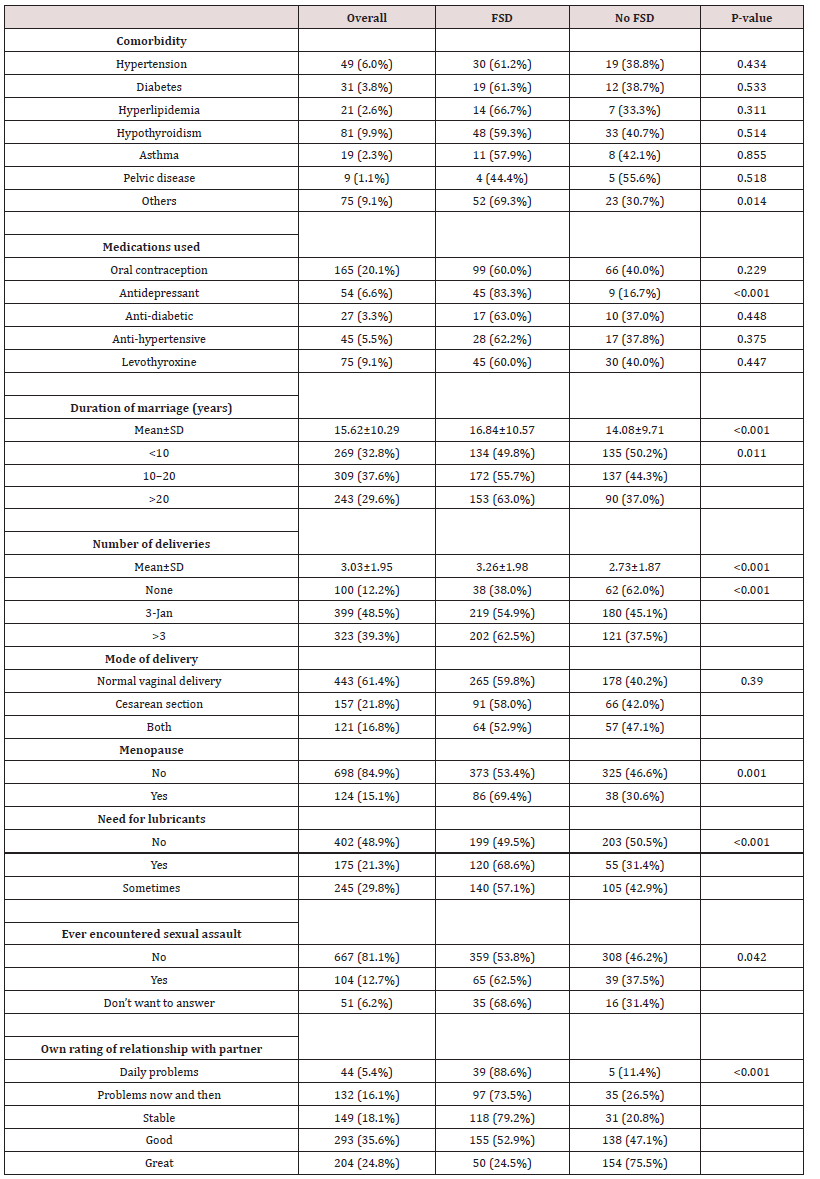
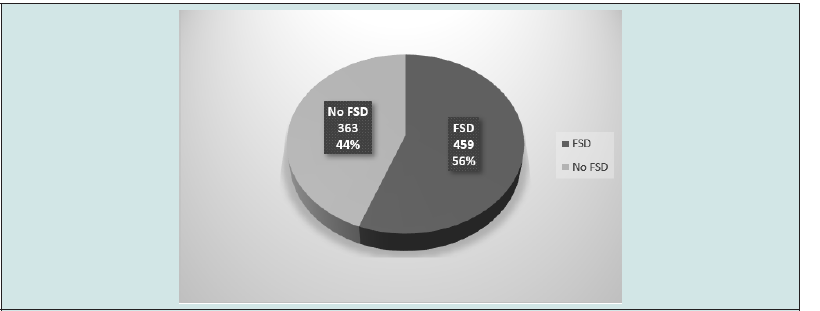
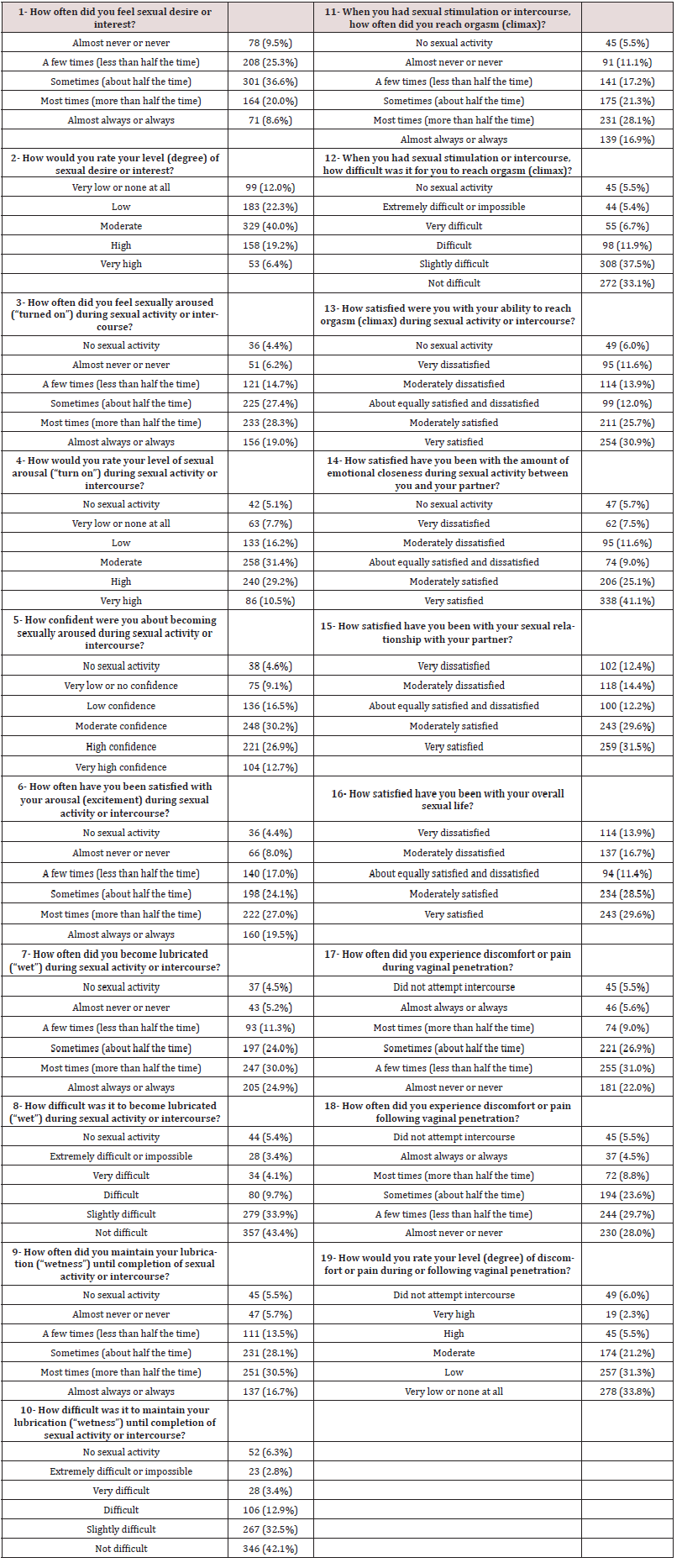
In total, 822 participants were included in the analysis and a total of 459 participants (55.8%) had FSD (FSFI ≤26.55). The details of the answers to the FSFI questions are provided in Supplementary Table 1 while Table 1 presents the demographic characteristics. Approximately 40% of the participants were between 36 and 45 years of age, with 36.4% aged ≤35 years and 23.6% aged ≥46 years. The majority (85.4%) of the participants had either a university degree (61.2%) or a postgraduate degree (24.2%). Most (61.6%) of the participants worked, with an average of 26.8±18.0 hours per week, and most (61.9%) of the working participants had a high amount of physical and emotional pressure at work. More than two-thirds (79.8%) of the participants’ partners had either a university degree (54.5%) or a postgraduate degree (25.3%). Approximately 38.9% of the participants had a family monthly income between 15,000 and 30,000 (SAR), with 29.2% earning <15,000 and 31.9% earning >30,000. The majority of participants were Saudi (93.7%) and more than half were residents of the central region (52.7%). The average Body Mass Index (BMI) was 27.0±5.2, with approximately one-quarter (25.1%) being obese (BMI ≥30). FSD was positively associated with increasing age (p=0.045), obesity (p=0.010), and a lower partner’s education level (p=0.007), but negatively associated with living in the eastern region (p=0.021). Table 2 shows the medical, marital, and sexual histories. Approximately 12.3% of participants had comorbidities, mainly hypothyroidism (9.9%), hypertension (6.0%), and diabetes (3.8%). Approximately 39.4% of the participants used medications, mainly oral contraception (20.1%), levothyroxine (9.1%), antidepressants (6.6%), and antihypertensive medications (5.5%). The average duration of marriage was 15.6±10.3 years, with 37.6% between 10 and 20 years.
The average number of deliveries was 3.0±2.0, with 48.5% having between one and three deliveries. Approximately 38.6% of the participants had a cesarean section, either alone (21.8%) or with (16.8%) normal vaginal delivery. Approximately 15.1% of the participants were menopausal. Approximately half of the participants used lubricants either sometimes (29.8%) or always (21.3%). Of the participants, 12.7% had encountered sexual assault and 6.2% refused to answer this question. The majority (60.5%) of participants reported a good or great relationship with their partner, 21.4% had problematic relationships, and 18.1% had a stable relationship. FSD was significantly associated with taking medications, especially antidepressants (p<0.001), a longer duration of marriage (p<0.001), higher number of deliveries (p<0.001), menopause (p=0.001), need for lubricants (p<0.001), encountering sexual assault (p=0.042), and a lower rating of their relationship with their partner (p<0.001). Table 3 lists the total and domain scores of the FSFI. The overall mean FSFI score was 24.10±7.20 points, representing 0.67%±0.20% of the maximum possible score. As expected, the overall FSFI score was significantly lower in those who had FSD than in those who did not (19.35±6.16 versus 30.11±2.18, p<0.001). The same pattern was observed in all FSFI domains (p<0.001). The domain with the lowest score was desire (3.47±1.22), followed by arousal (3.76±1.48), orgasm (4.04±1.61), pain (4.24±1.54), satisfaction (4.24±1.60), and lubrication (4.35±1.39). Table 4 shows the multivariate logistic regression model of potential predictors of FSD. Out of all variables that were associated with FSD in Tables 1 and 2, the following were independent predictors of FSD (listed in descending order according to the Odds Ratio [OR]): use of antidepressants (3.12), always need to use lubricants (2.26), undisclosed sexual assault history (2.16), both cesarean section and vaginal delivery (2.05), lower level of partner’s education (1.99), menopause (1.70), sometimes need to use lubricants (1.47), and residence in the central region (1.43) (Table 5).
Table 3: Total and domain scores for the Female Sexual Function Index (FSFI) by female sexual dysfunction status (N=822).
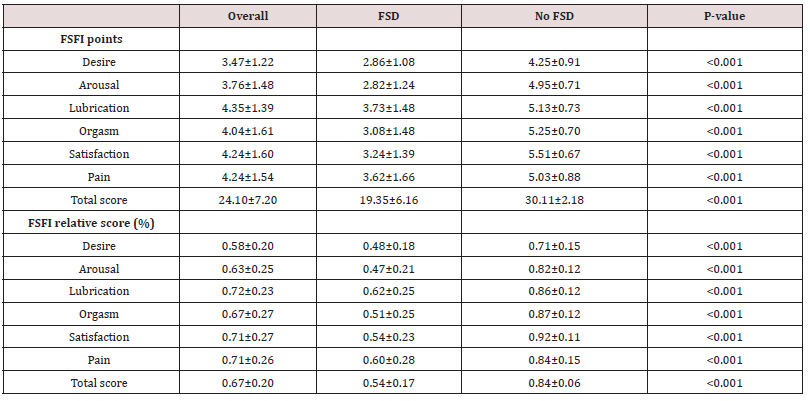
Table 4: Multivariate logistic regression model* of potential predictors of female sexual dysfunction (N=822).
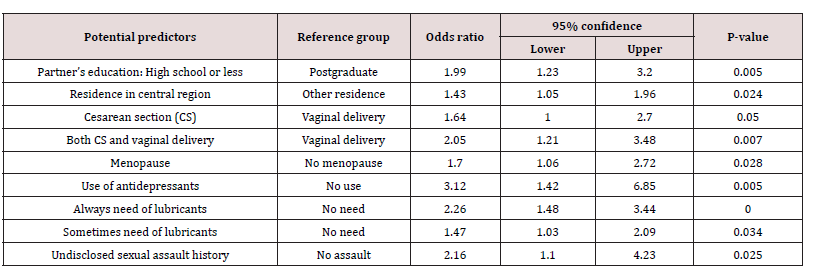
* Adjusted for variables associated with female sexual dysfunction in Tables 1 and 2 (p<0.10). Backward elimination was used to allow non-significant variables to leave the model. R-square = 0.257.
Table 5: Supplementary Table 1: Responses to the questions of the Female Sexual Function Index (N=822).
Discussion
In this study, we collected and analyzed epidemiological data on the prevalence and predictors of FSD in a sample of Saudi women. Of the 822 participants who were included, 459 (55.8%) had FSD (FSFI ≤26.55). This high prevalence is consistent with reports from China [3], Japan[10], Egypt[11], and Jordan[12]. Its prevalence was lower in the USA [7], Austria[13], and Turkey[14, 15]. Fluctuations in prevalence among different regions are often due to multiple reasons. For example, FSD can be associated with age; socioeconomic status; degree of education; employment; biological, medical, and psychological factors; the clinical definition used for each dysfunction; and the criteria of samples examined (general population vs. hospitals or specialized clinics)[3, 6]. The total and domain scores of the FSFI are shown in Table 3. The overall FSFI score was 24.10±7.20 points, representing 0.67%±0.20% of the maximum possible score. As expected, the overall FSFI was significantly lower in those who had FSD than in those who did not (19.35±6.16 versus 30.11±2.18, p<0.001). The same pattern was observed in all FSFI domains (p<0.001). The domain with the lowest score was desire (3.47±1.22), followed by arousal (3.76±1.48), orgasm (4.04±1.61), pain (4.24±1.54), satisfaction (4.24±1.60), and lubrication (4.35±1.39). This was expected, as most literature reported desire and arousal disorders to be the most frequently reported female sexual disorders[1, 5, 7, 13, 16]. Similar results were reported by Madbouly et al. in a study that included 200 Saudi women [5] and by Aslan et al. in a study that included 1, 009 Turkish women[15]. Laumann et al. reported sexual desire problems in 22% of women, arousal problems in 14%, and sexual pain in 7% [7]. Moreover, a study by Oberg et al.[16] showed that 45% of Swedish women had a reduced desire. Studies have highlighted that the risk factors for FSD are age, medical history of sexually transmitted diseases, pelvic floor disorders and pelvic surgeries, depression, history of sexual abuse, lower educational attainment, socioeconomic status, physical health, lifestyle, and sexual experience[5, 7, 12]. In our study, FSD was associated with increasing age (p=0.045), menopause (p=0.001), obesity (p=0.010), lower level of partner’s education (p=0.007), duration of marriage (p= 0.001), number of deliveries (p< 0.001), and partner relationship status (p=0.001) (Tables 1 & 2). Out of all variables that were associated with FSD, there were independent predictors of FSD, such as use of antidepressants (OR 3.12), always need to use lubricants (OR 2.26), undisclosed sexual assault history (OR 2.16), both cesarean section and vaginal delivery (OR 2.05), lower level of partner’s education (OR 1.99), menopause (OR 1.70), sometimes need to use lubricants (OR 1.47), and residence in the central region (OR 1.43).
Madbouly et al. showed that being > 40 years of age increases the FSD risk by approximately 5 times [5]. The International Women’s Survey on Health and Sexuality studied participants from the United States and different regions of Europe (France, Germany, Italy, and the United Kingdom) aged between 20 and 70 years and reported that sexual activity decreased with age and the proportion of women with low sexual function, specifically low desire, increased with age[17, 18]. Likewise, Abduljabbar et al. reported a significantly greater risk of FSD in patients aged >40 years in a group of 194 Saudi women using an abridged 6-item version of the FSFI [19]. Similarly, a study conducted in Turkey by Oksuz et al. reported that at ages 31 to 45 years, sexual dysfunction increased with an OR of 2.1; further, menopause was associated with a 2-fold higher risk of sexual dysfunction, and even the OR was 1.7-fold higher [14]. This study showed that menopause was associated with a higher risk of sexual dysfunction (odds ratio [OR] = 1.70). Lower sexual function with age can be explained by age-associated physiological changes in hormones, psychosocial factors, medication use, and associated comorbidities [20]. In addition, Avis et al. noticed that menopause is related to lower sexual desire but not all aspects of sexual functioning [21]. In contrast, Gonzalez et al. stated that menopause slightly decreased all stages of sexual function, but this association was significant only for the lubrication and pain domains[22]. The results of studies investigating education level as a risk factor varied. Some reports have found no relationship[5,8,11], while others have shown that a lower educational level is associated with a higher risk of FSD [7,23]. Laumann et al. reported that low socioeconomic status and a low level of education were risk factors for FSD [7]. Our findings showed that lower sexual function was more common with a lower level of partner education (OR 1.99). The female educational level was not significantly related to FSD risk in our participants (p = 0.452) or low socioeconomic status (p = 0.248). Unfavorable social conditions and economic stress were among the aggravating factors for sexual problems in 28.1% of respondents in a study conducted in lower Egypt [24]. Madbouly et al. showed that low sexual function is more common in women with a lower family income (OR 6.06), and they attributed this to the associated female stress, anxiety, and depression [5]. In our study, a longer duration of marriage was significantly associated with a higher risk of FSD (p<0.001), as well as the number of deliveries (p<0.001). No significant differences were detected owing to the duration of marriage in a study by Madbouly et al. [5]; Aslan et al. [15] found similar results in a study of 1,009 Turkish women. Depression and antidepressants are major risk factors for FSD [25]. A substantial percentage of patients experience some disturbance in sexual function while taking antidepressants. A meta-analysis that assessed rates of adverse sexual effects concluded that the rate of sexual dysfunction attributable to antidepressants was approximately 40% and the rate of sexual dysfunction associated with placebo was approximately 14% [26]. In our study, antidepressants were significantly associated with a higher risk of FSD (p<0.001). FSD is an under investigated health challenge. As mentioned earlier, many women in Saudi culture are shy or hesitant to discuss their sexual health concerns with healthcare providers. Published reports on the risk of FSD in Saudi Arabia are limited. This study has the advantages of including a large community-based sample size and the use of the validated ArFSFI. Other studies used either a non-validated Arabic version [27,28], an abridged 6-item version of the FSFI [19], or surveyed special populations with a smaller number such as Saudi women with type 2 diabetes [29], health care providers [30], or Saudi women attending primary care and gynecology clinics at a teaching hospital in a specific region [5].
Thus, our results can be generalized to the entire community with relative confidence. However, male partners were not evaluated regarding their sexual performance, and data on their sexual abilities were not obtained from their female partners because it might be biased or inaccurate (Figure 1).
Conclusion
In this study, we estimated the prevalence of FSD in Saudi women using a validated instrument (the FSFI). The prevalence of FSD in Saudi Arabia is 56%. Desire and arousal were the most significantly affected domains, followed by orgasmic problems. The most significant risk factors for FSD are the use of antidepressants, older age, menopause, obesity, and marriage duration. More studies with structured interviews with both partners regarding risk factors and predictors are strongly warranted. Overall, this study addressed a critical health problem that has not been adequately studied in the community. The high prevalence of FSD deserves attention as it is a major public health concern. We need to increase the knowledge and experience of physicians regarding FSD so that they can approach women with such problems professionally. The use of the full-version ArFSFI for assessing women in clinical settings by family physicians, obstetricians, and gynecologists, or psychologists and research settings is strongly recommended for better standardization and comparison.
Author Contributions:
Maysoon AlHaizan contributed to project development, data collection, and manuscript writing/ editing. Ghada AlGudairi contributed to questionnaire building, data collection, data analysis, and results writing/editing. Dana AlDabeeb contributed to data collection, manuscript review and editing. Maha Alhainiah contributed to data collection, manuscript review and editing. Rahaf AlHarthi data collection. Saleh Binsaleh contributed to manuscript review and editing. Ghadeer AlShaikh contributed to protocol/ project development, data collection, and manuscript review and editing.
Acknowledgments:
We thank Prince Naif Health Research center, Investigator support unit at King Saud University.
Conflict of Interest:
The authors declare no conflict of interest.
Funding:
None.
Data Availability Statement:
This is an open access article under the CC BY-NC-ND license ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ).
References
- McCool ME, Theurich MA, Apfelbacher C (2014) Prevalence and predictors of female sexual dysfunction: a protocol for a systematic review. Systematic reviews 3(1): 1-5.
- Ahmed Al Badr, Rafeef Al Juraifani, Ghadeer Al Sheikh, Hazem Al Mandeel, Lateefa Al Dakhyel, et al. (2017) Validation of the International Urogynecology Association’s pelvic organ prolapse/urinary incontinence sexual questionnaire in Arabic. International urogynecology journal 28(3): 437-445.
- Wen Jia Lou, Bo Chen, Lan Zhu, Shao Mei Han, Tao Xu, et al. (2017) Prevalence and factors associated with female sexual dysfunction in Beijing, China. Chinese medical journal 130(12): 1389-1394.
- First MB, Wakefield JC (2013) Diagnostic criteria as dysfunction indicators: bridging the chasm between the definition of mental disorder and diagnostic criteria for specific disorders. The Canadian Journal of Psychiatry 58(12): 663-669.
- Khaled Madbouly, Mohammed Al Anazi, Hanan Al Anazi, Abdullah Aljarbou, Raed Almannie, et al. (2021) Prevalence and predictive factors of female sexual dysfunction in a sample of Saudi women. Sexual Medicine 9(1): 100277.
- Gamal El Atrash, Mohamed H Ali, Hassan A Abdelwahab, Lobna A Abdelreheem, Mostafa Shamaa (2014) The assessment of sexual dysfunction in Egyptian women with lower urinary tract symptoms. Arab journal of urology 12(3): 234-238.
- Laumann EO, Paik A, Rosen RC (1999) Sexual dysfunction in the United States: prevalence and predictors. Jama 281(6): 537-544.
- Rosen CB, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. (2000) The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. Journal of sex & marital therapy 26(2): 191-208.
- Tarek H Anis, Samah Aboul Gheit, Hanan S Saied, Samar A Al kherbash (2011) Arabic translation of Female Sexual Function Index and validation in an Egyptian population. The journal of sexual medicine 8(12): 3370-3378.
- Shin ichi Hisasue, Yoshiaki Kumamoto, Yoshikazu Sato, Naoya Masumori, Hiroki Horita, et al. (2005) Prevalence of female sexual dysfunction symptoms and its relationship to quality of life: a Japanese female cohort study. Urology 65(1): 143-148.
- Ibrahim ZM, Ahmed MR, Ahmed WAS (2013) Prevalence and risk factors for female sexual dysfunction among Egyptian women. Archives of gynecology and obstetrics 287(6): 1173-1180.
- Maher Elias Maaita, Basel M Khreisat, Omar A Tasso, Nareman Naser Otom, Bayan M Aljaafreh, et al. (2018) Prevalence and associated risk factors of female sexual dysfunction among Jordanian women. Journal of family medicine and primary care 7(6):1488-1492.
- Anton Ponholzer, Michaela Roehlich, Ursula Racz, Christian Temml, Stephan Madersbacher (2005) Female sexual dysfunction in a healthy Austrian cohort: prevalence and risk factors. European urology 47(3): 366-375.
- Oksuz E, Malhan S (2006) Prevalence and risk factors for female sexual dysfunction in Turkish women. The Journal of urology 175(2): 654-658.
- Ergul Aslan, Nezihe Kizilkaya Beji, Ilkay Gungor, Ates Kadioglu, Birsen Kucuk Dikencik (2008) Prevalence and risk factors for low sexual function in women: a study of 1,009 women in an outpatient clinic of a university hospital in Istanbul. The Journal of Sexual Medicine 5(9): 2044-2052.
- Öberg K, Fugl-Meyer A, Fugl-Meyer KS (2004) On categorization and quantification of women's sexual dysfunctions: an epidemiological approach. International Journal of Impotence Research 16(3): 261-269.
- Richard D Hayes, Catherine M Bennett, Christopher K Fairley, Lorraine Dennerstein (2006) Epidemiology: What can prevalence studies tell us about female sexual difficulty and dysfunction? The journal of sexual medicine 3(4): 589-595.
- Graziottin A (2007) Prevalence and evaluation of sexual health problems-HSDD in Europe. The journal of sexual medicine 4: 211-219.
- Abduljabbar HSO, Alkasih MA, Khayat SW, Qotbi RM, Alkhatieb MT, AbduljabbarAH, et al. (2016) Screening of sexual dysfunction in Saudi women before and after the age of 40 years. Clinical and Experimental Obstetrics & Gynecology 43(4): 526-528.
- Basson R, Berman J, Burnett A, Derogatis L, Ferguson D, et al. (2000) Report of the international consensus development conference on female sexual dysfunction: definitions and classifications. The Journal of urology 163(3): 888-893.
- Avis NE, Stellato R, Crawford S, Johannes C, Longcope C, et al. (2000) Is there an association between menopause status and sexual functioning? MENOPAUSE (5): 297-309.
- Marcela González, Gloria Viáfara, Fresia Caba, Esteban Molina (2004) Sexual function, menopause and hormone replacement therapy (HRT). Maturitas 48(4): 411-420.
- Selahittin Cayan, Erdem Akbay, Murat Bozlu, Bülent Canpolat, Deniz Acar, et al. (2004) The prevalence of female sexual dysfunction and potential risk factors that may impair sexual function in Turkish women. Urologia internationalis 72(1): 52-57.
- Elnashar AM, EL Dien Ibrahim M, EL Desoky MM, Ali OM, Elayd Mohamed Hassan M (2007) Female sexual dysfunction in Lower Egypt. BJOG: An International Journal of Obstetrics & Gynaecology 114(2): 201-206.
- Lorenz T, Rullo J, Faubion S (2016) Antidepressant-induced female sexual dysfunction. in Mayo Clinic Proceedings 91(9): 1280-1286.
- Reichenpfader U, Gartlehner G, Morgan LC, Greenblatt A, Nussbaumer B, et al. (2014) Sexual dysfunction associated with second-generation antidepressants in patients with major depressive disorder: results from a systematic review with network meta-analysis. Drug safety 37(1): 19-31.
- Alsibiani SA, Rouzi AA (2010) Sexual function in women with female genital mutilation. Fertility and sterility 93(3): 722-724.
- Alsibiani SA (2014) Effects of pregnancy on sexual function. Findings from a survey of Saudi women. Saudi medical journal 35(5): 482-487.
- Turki A AlMogbe, Hussein S Amin, Saad M AlSaad, Turky H AlMigbal (2017) Prevalence of sexual dysfunction in saudi women with Type 2 diabetes: Is it affected by age, glycemic control or obesity?. Pakistan journal of medical sciences 33(3): 732-737.
- Abdulrahim A Rouzi, Nora Sahly, Dana Sawan, Souzan Kafy, Faten Alzaban (2015) The prevalence of sexual dysfunction in the female health care providers in Jeddah, Saudi Arabia. Scientific Reports 5(1): 1-3.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...