Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Review Article(ISSN: 2637-4544) 
Modern Contraception Choices Among Family Planning Clients in A Nigerian Tertiary Hospital: A 5-Year Retrospective Cross-Sectional Study Volume 5 - Issue 2
Odigonma Zinobia Ikpeze1, Chukwuemeka Chukwubuikem Okoro1*, George Uchenna Eleje1,2, Golibe Christian Ikpeze1, Tobechi Kingsley Njoku1, Chigozie Geoffrey Okafor1, Richard Obinwanne Egeonu1, Samuel Okwuchukwu Ilikannu3, Amarachukwu Doris Okoro4, JohnBosco E Mamah 5 and Okechukwu Christian Ikpeze1,2
- 1Department of Obstetrics and Gynaecology, Nnamdi Azikiwe University Teaching Hospital, Nnewi, Anambra State, Nigeria
- 2Department of Obstetrics and Gynaecology, Nnamdi Azikiwe University Awka, Anambra State, Nigeria
- 3Department of Obstetrics and Gynaecology, Federal Medical Centre, Asaba, Delta State, Nigeria
- 4College of Nursing, Nnamdi Azikiwe University Teaching Hospital Nnewi, Anambra State, Nigeria
- 5Department of Obstetrics and Gynecology, Alex Ekwueme Federal University Teaching Hospital, Abakaliki, Nigeria
Received:June 24, 2023;Published:June 28, 2023
Corresponding author:Chukwuemeka Chukwubuikem Okoro, Department of Obstetrics and Gynaecology, Nnamdi Azikiwe University Teaching Hospital, Nnewi, Anambra State, Nigeria
DOI: 10.32474/IGWHC.2023.05.000222
Abstract
Background:Contraception is very critical in reducing unwanted pregnancies and plays a key role in preventing maternal mortality, lowering preterm delivery, and reducing neonatal and infant deaths. Despite attempts by the government and nongovernmental organizations to boost its use, the uptake of contraception in Nigeria has remained low.
Objective: To determine the prevalence and pattern of uptake of modern contraception by family planning clients.
Methods:This is a five-year retrospective cross-sectional study of modern contraception services in Nnamdi Azkiwe University Teaching Hospital (NAUTH), Nnewi, Nigeria between January 1st 2017 and 31st December 2021. Participants’ file numbers were obtained from the registers in the family planning clinic and theatres. The case files were retrieved from the medical records department and available participants’ information was obtained and recorded in proformas. The outcome measures were the contraceptive prevalence rate and the method of contraception used. The data was analysed using the statistical product and service solutions (SPSS) computer software version 26.0 IBM Corporation.
Results: Within the study period, 3,638 deliveries were conducted, while 723 clients had contraception, giving an overall contraceptive prevalence rate of 19.9%. The modal age range of women who used contraception was 30 to 34 years (31.7%). The most frequently used method of contraception was the Levonogestrel containing implant (Jadelle) which was used by 44.2% of the clients. Only 2.3% of the clients had bilateral tubal ligation (BTL), while there was no recorded case of vasectomy. Most of the clients (89.0%) were in a marriage relationship.
Conclusion:The uptake of contraception is on the increase; however, it is still below the acceptable level. There is a need for promotion of sexual and reproductive health education to improve the usage of contraception.
Keywords:Contraception; contraceptive; contraceptive prevalence; family planning; Nigeria
Introduction
Contraception is the prevention of unwanted pregnancies. Contraceptives are agents, drugs or devices that are used to prevent unintended pregnancies [1]. Contraception is an essential component of maternal, child health, and reproductive therapies because it plays a variety of functions in preventing maternal mortality, lowering preterm delivery, and reducing neonatal and infant deaths [2]. Modern contraception methods include products or medical procedures that interfere with reproduction from acts of sexual intercourse [3]. These methods do not require couples to avoid sex, or use a different method, on specific days of the menstrual cycle. Worldwide, issues related to pregnancy or delivery kills about 830 women per day. More than 59,000 women lose their lives to childbirth and complications from unintended pregnancies each year in Nigeria, which has a high fertility rate of 5.5 children per woman (the second highest in the West African region and the 13th in the world) [4], a high fecundity rate, and a population that exceeds 170 million with an estimated growth rate of 3.2% per year. Effective contraception is very critical to reducing unwanted pregnancies and the associated problems as well as ensuring that men and women enjoy their sexual and reproductive lives with little or no risks of pregnancy [3,5]. Maternal mortality is a scourge and is still ravaging the developing countries, especially sub- Saharan African countries unlike in developed countries where it has been at an irreducible minimum [6]. Nigeria accounts for about 10% of the global maternal mortality rate (MMR) with abortions accounting for 20%–40% of maternal mortality in the countr [7]. Nigeria’s MMR has not significantly decreased, according to data from the National Demographic and Health Survey (NDHS), which was conducted between 2008 and 2018, (545,576 and 512 deaths per 100,000 live births). This is not in line with the SDG 3.1 target of decreasing MMR globally to as minimum as 70 deaths per 100,000 live births. But according to the 2018 NDHS only 12% of Nigerian women utilize a modern method of contraception, which leads to high rates of unintended or unexpected births and unsafe abortions [8]. High rates of fertility, maternal mortality, and infant mortality are common in low- and middle-income nations, and they are frequently caused by inadequate use of contraception. In these nations, an estimated 214 million women of reproductive age wanted to avoid getting pregnant in 2018 but did not use contraception [9]. Majority of married women who did not want any more children do not use effective contraception. Reproductive health services like family planning, antenatal care, safe delivery, and emergency obstetric care have all been identified as interventions to combat maternal mortality in developing countries. Despite attempts by the government and non-governmental organizations to boost its use, the rate of usage of contraception in Nigeria remains low at 22.7% [10,11]. This low rate of contraceptive use in sub- Saharan Africa and Nigeria has been attributed to socioeconomic situation, educational attainment, religious and cultural influences, and a lack of understanding of contraception [12]. The Sustainable Development Goals (SDGs), target 3.7 expects countries to “ensure universal access to sexual and reproductive health-care services, including for family planning, information and education, and the integration of reproductive health into national strategies and programmes” by 2030 [13]. It is imperative that periodically, progress towards this target should be assesses by monitoring key family planning indicators, including the range and types of contraception used.
According to recent data from Performance Monitoring for Action (PMA) surveys, unmarried women tend to choose shortacting methods including male condoms (56.6% of users), oral contraceptive pills (25.2%), and emergency contraception (8.4%) while married women chose male condoms (20.1%), oral contraceptives (23.0%), and injectable contraceptives (30.2%) [14].
The promotion of family planning and access to modern contraception has the potential to reduce poverty, hunger, slow population growth, reduce unwanted pregnancies, and lower the cost of meeting sustainable development goals, such as achieving universal primary education, which is influenced by the number of children in need of education; decrease injuries, illness, and deaths related to childbirth and abortion; prevent sexually transmitted infections, such as HIV; and reduce or eliminate unwanted pregnancies, improve life expectancy and decreasing the dependency rate with preservation of the environment [15]. By utilizing contemporary contraception, women of reproductive age are free to choose for themselves if, when, and how many children they wish to have. This helps to achieve Sustainable Development Goals (SDGs) 3 and 5, which are about excellent health and wellbeing and gender equality respectively [12]. In addition to these negative social and economic effects, unintended pregnancies can cause girls, their families, and society to fall short of their potential in terms of academic success and struggle to find gainful employment, which frequently traps them in a cycle of poverty [16]. The importance of contraception in modern gynecological practice cannot be overemphasized. Unintended pregnancy poses a major health challenge to reproductive health. About 36% of pregnancies are unplanned leading in most cases to criminal abortion and maternal deaths. This study was carried out to determine the uptake of modern contraception, the pattern of usage as well as method preferences among women attending the family planning clinic in a low and middle-income country.
Materials and Methods
Study Design
This is a five-year retrospective cross-sectional study of modern contraception choices among couples who had contraception.
Study Population
The study was conducted among couples who chose any form of modern contraception from 1st January 2017 to 31st December 2021.
Study Setting
This study was conducted in the family planning clinic, obstetric/labour ward and theatre of Nnamdi Azikiwe University Teaching Hospital, Nnewi, Nigeria. The hospital is a 400 bedded tertiary institution located in Anambra State, Southeastern Nigeria. The hospital serves the inhabitants of Nnewi, a semi urban settlement and its surrounding towns, it has a non-selective policy towards antenatal cases.
Eligibility Criteria
The study included women who used modern method of contraception with their partners during the study period (from 1st January 2017 to 31st December 2021). Women who had traditional method of contraception or who did not use contraception were excluded from the study. The cases of missing or incomplete data were also excluded from the study.
Sample Size Determination
It was an all population-based study.
Study Outcome Measures
The outcomes examined in the present study included contraceptive prevalence rate and contraception choices/methods.
Sample Technique and Procedure
Non-random sampling approach was adopted for the study. All available relevant case files from the medical record department were examined. The family planning, labour ward and obstetric theatre delivery registers were used to extract information on the total number of deliveries, number of women who attended the family planning clinic and women who had post-partum bilateral tubal ligation over the 5-year period. Their case files were retrieved from the medical records department. The participants’ sociodemographic variables, contraception choices were retrieved from the participants’ case files using proformas.
Statistical Analysis
The data was analyzed using the Statistical Product and Service Solutions (SPSS) computer software version 26.0 IBM Corporation.
Ethical Approval
Informed consent was not sought for the present study because it was a retrospective study of cases. However, ethical approval was obtained (Reference No. NAUTH/CS/66/Vol.15/ VER.3/140/2022/104.). The study was conducted according to the Helsinki declarations on ethical principles for medical research involving human subjects.
Result
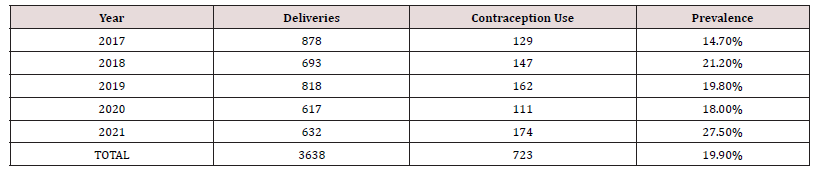
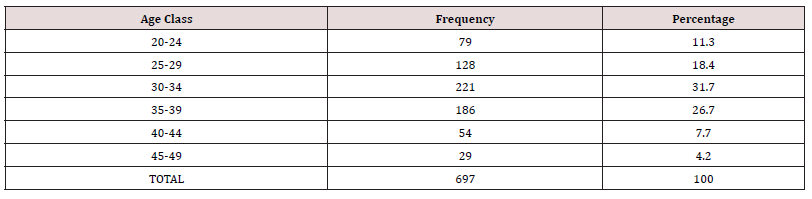
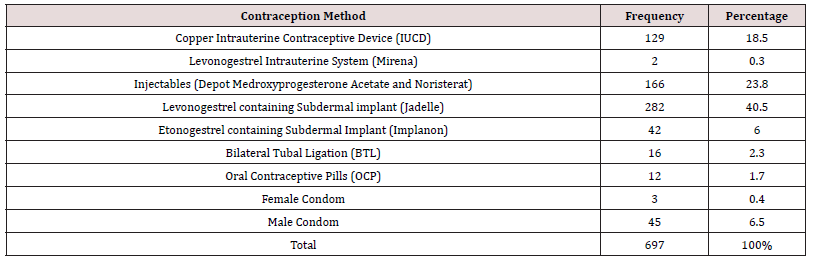
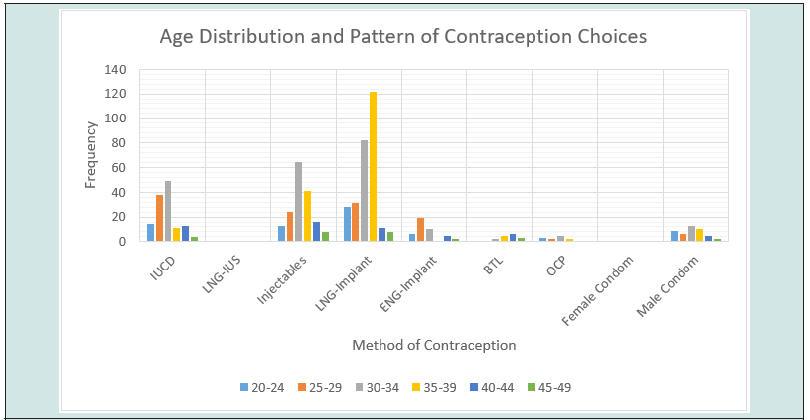
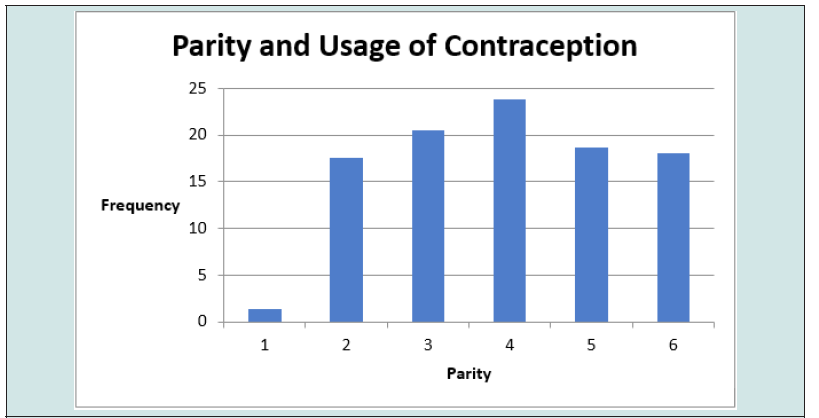
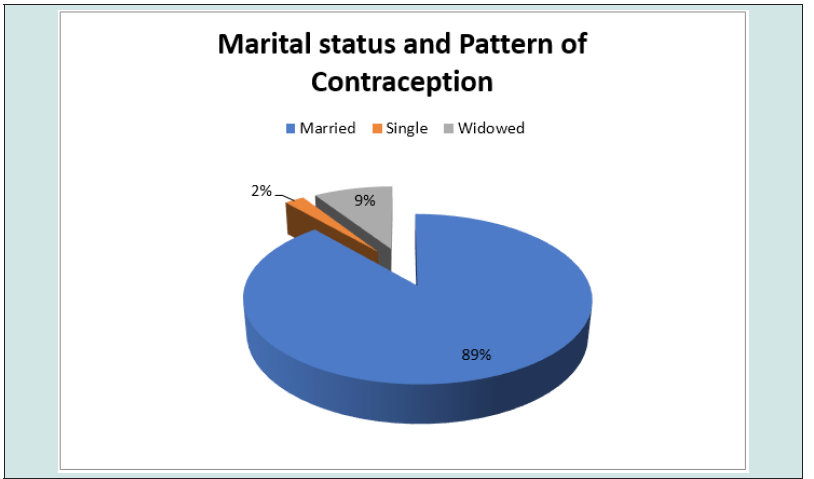
The total number of deliveries at NAUTH, Nnewi in the studied period was 3,638, while the total number of clients who used contraception was 723, giving an overall contraceptive prevalence rate of 19.9%. Out of the 723 clients who received contraception, only 697 were retrieved with complete information in their case notes giving a retrieval rate of 96.4% and were used for further analysis. Table 1 shows the prevalence rate of contraception use over a 5-year study period. Overall, there was a rise in the pattern of contraception usage as well as prevalence during the study period, showing a rise from 14.7% in 2017 to 27.5% in 2021. The use of contraception increased steadily from a total of 129 in 2017 to 174 in 2021. The age distribution and contraception usage of the clients is shown in Table 2 and Figure 1. The age range of the clients was from 20 to 49 years. The modal age range of women was 30 to 34 years (31.7%), followed by 35 to 39 years (26.7%). Table 3 shows the frequency of usage of the different methods of contraception. The most frequently used method of contraception was the Levonogestrel containing implant (Jadelle) (44.2%), followed by the injectables (Depot Medroxyprogesterone Acetate and Noristerat) (23.8%) and then the copper containing intrauterine contraceptive device (18.5%). Levonogestrel containing intrauterine system (Mirena) and female condom both had a usage of less than 1% each while male sterilization, hormonal patches, diaphragms and cervical caps, spermicidal agents (gels, foams, creams, suppositories, etc.) or vaginal rings was not used by any of the couples. Most of the clients that used contraception have had four deliveries or more. This is shown in Figure 2. Figure 3 shows the relationship between pattern of contraception usage and marital status. A great number of the clients (89.0%) were married, while 9.0% widowed and 2.0% were single.
Discussion
The overall contraceptive prevalence rate in relation to
deliveries at the hospital over the period of study was 19.9%, which
showed improvement from a previous study done in the study
centre which showed a prevalence of 12.8% [17]. This prevalence
is comparable to findings of other studies done in Lagos, Nigeria
and DR Congo which showed a prevalence of 16.7% and 16.2%
respectively [18]. This was, however, lower than a prevalence of
42.6% reported in Kenya [19] and 43% reported in Zambia [20].
Cultural barriers, religion, cost of the method, husband/partner’s
refusal, fear of possible side effects, superstition, misinformation,
and desire for large family’s size have been identified as factors
contributing to low usage of family planning services [4,17].
Ugboaja et al, in their Nigerian study reported that fear of family
planning commodities interfering with future fertility was the
commonest reason for non-use of contraception in their study [5].
The highest prevalence of contraceptive uptake in the study was
in 2021 with prevalence of 27.5% followed by 2018 at 21.2% and
2019 at 19.8% (Table 1). The overall rise in the prevalence rate of
contraception usage from 14.7% in 2017 to 27.5% in 2021 could be
due to an increasing knowledge and demand for contraception use
among women. It is important to note that there was a slight decline
in the trajectory in 2020 which could be because of the COVID-19
pandemic as seen in a similar study [21]. The study showed that
the subdermal implants were the most used contraception method
amongst women attending the family planning clinic in NAUTH
during the 5-year study period, accounting for 46.5%. This was
like other studies done in Ibadan, Nigeria [22] and United States of
America [23] which showed preference for implants. This however
was in contrast to a study done in Kano [24], Northern Nigeria
where injectables were the most preferred options and previous
studies done in the study centre, [17] in Asaba, Nigeria [25] and
Ibadan, Nigeria [26] where intrauterine contraceptive device was
most preferred option. The reason for the choice of implants may be
because they are long-acting contraceptives and the fact that they
do not require repeated hospital visits. Also implants in the last 2
years of the study were noted to have gained preference over other
contraception methods, possibly due to better knowledge of the
contraception method of client population within the study area.
This contraception method may be fulfilling an unmet need for a
long-acting reversible method of contraception for women who
have achieved their desired family size but for fear of the unknown
do not want sterilization. A United Nations document has reported
that female sterilisation is the most common contraception method
used worldwide [13]. This is contrary to the findings of our study,
where only 16 (2.3%) women had BTL. All of them who had BTL
had it as part of caesarean section either due to a desire to limit
family size or as part of the management of uterine rupture and
a means of preventing a repeat uterine rupture should pregnancy
occur. None of the women had interval BTL. There is poor uptake
of interval BTL.
This may relate to superstition that women who accept tubal ligation are born with blocked tubes in their next life [17]. The study shows unsatisfactory role of males in contraception. Only 45 (6.5%) of the clients made use of male condom with their partners. Generally, African males dislike the condom. No one had vasectomy as a form of family planning during the period under review. Men abhor vasectomies and some have even attributed it to impotence later in life and infertility in their next lives. Further enlightenment among the male folks is needed to improve their acceptance and usage of contraception. Most of the clients fall into the age group 30 to 34 (32.8%) years. This was like the finding in a study by Akinloye et al [26] with the commonest age group of 30 to 39 years. The second most common age group was 35 to 39, 174 (27.2%) years. A plausible reason for this finding could be that older women would have given birth and completed their family size, increasing their likelihood of using contraception to prevent any unintended pregnancy. Women aged 25 to 39 years made use of contraception more readily than the women at the extremes of the age groups in this study. This is comparable to other studies [11]. This is not surprising as they are within the prime of the reproductive age. These women preferred long-acting reversible contraceptive methods like intrauterine contraceptive device (IUCD), injectables and implants. There was a very low uptake in the 45-49-year age group (4.2%), this is like a study in Yangon [27]. Lasong et al also reported that the age range of 40-49 years was negatively associated with contraception use compared with young age [20]. The finding may be attributed to lower fecundity and reduced sexual activity in this age group [20]. The study shows that most (89%) of the clients were in a marriage relationship, 63 (9%) were widowed while 14 (2%) were single. The significant difference in contraception use between married and unmarried women agrees with findings of other studies whereby more married women have been observed to have the need for family planning than single women [19,28,29].
Women who had four or more children were more likely to use modern contraception compared to those with no children. Similar findings were observed in other previous studies [7]. A plausible reason for this finding could be that women with parity below three are at the peak of their childbearing period and would not want to consider using any contraception method until they have had their desired family size.The use of contraception can help in prevention of unwanted pregnancy and subsequent abortions [25]. If more women engage in contraception use, there will be a significant reduction in unwanted pregnancies and abortions which in turn would lead to a reduction in maternal morbidity and mortality. This can be achieved with proper counseling and education to encourage women on contraception usage and eradication of myths associated with contraception by increasing global access to information, communication, and technology. Overcoming these potential barriers will require innovative strategies such as including men and religious leaders in the discussion about family planning uptake including contraception [4]. A main strength of our study is the inclusion of records from theatre and family planning registers. Further, the use of theatre records limits inclusion bias as up to 2.2% of the women had bilateral tubal ligation. Limitations of our study include missing data, related to known difficulties in conducting retrospective studies. This may have introduced sampling/selection bias and the data may not be representative of the whole population of patients.
Conclusion
The findings in this study showed that there’s a rising trend in usage of contraception with the sub-dermal implants being the most used. However, contraception uptake is still below the acceptable level. Promotion of women sexual reproductive health education ought to be encouraged to improve usage of contraception. Continued efforts should be made to improve the awareness and utilization of these services to improve health and better population control. Considering the influence of religious leaders on their followers, stakeholders may target working with religious leaders in disseminating information about contraception. Due to the need for continuous follow up, contraception services help in early detection of benign and malignant uterine lesions and offer opportunities for counselling on other health matters.
Compliance with Ethical Standards
Acknowledgments: The authors would like to thank the
nurses, medical record staff and other hospital staff who helped in
generating and preserving the data used in this study.
Data Availability: The data used to support the findings of this
study are available from the site publicly.
Funding: The authors received no specific funds for this work.
Contribution to Authorship: Ikpeze OZ, Njoku TK and
Egeonu RO contributed to the conception of the study, design,
manuscript writing and revision. Ikpeze OZ, Okoro CC and Ikpeze
GC contributed to data collection, data analysis, manuscript writing
and revision. Eleje GU, Okafor CG, Ilikannu SO, Okoro AD, Mamah
JE and Ikpeze OC contributed to manuscript writing and revision.
All authors gave final approval of the version to be published and
agreed to be accountable for all aspects of the work.
Disclosure of conflict of interest: The authors declare that
they have no conflict of interest.
Statement of ethical approval: Informed consent was not
sought for the present study because it was a retrospective study
of cases. The study was approved by the ethics review board of
Nnamdi Azikiwe University Teaching Hospital, Nnewi, Nigeria
(Reference No. NAUTH/CS/66/Vol.15/VER.3/140/2022/104.).
The study was conducted according to the Helsinki declarations on
ethical principles for medical research involving human subjects.
References
- Nkemakolam HC, Olanrewaju SO (2020) Trend and Determinant of Contraceptive Use Among Women of Reproductive Age in Nigeria. African J Math Stat Stud 3(2):14-36.
- Asaolu I, Nunõ VL, Ernst K, Taren D, Ehiri J (2019) Healthcare system indicators associated with modern contraceptive use in Ghana, Kenya, and Nigeria: Evidence from the Performance Monitoring and Accountability 2020 data. Reprod Health 16(1):152.
- Hubacher D, Trussell J (2015) A definition of modern contraceptive methods. Contraception 92(5): 420-421.
- Adefalu AA, Ladipo OA, Akinyemi OO, Popoola OA, Latunji OO, et al. (2019) Qualitative exploration of factors affecting uptake and demand for contraception and other family planning services in north-west Nigeria. Afr J Reprod Health 23(4): 63-74.
- Ugboaja JO, Nwosu BO, Ifeadike CO, Nnebue CC, Obi-Nwosu AI (2011) Contraceptive Choices and Practices among Urban Women in Southeastern Nigeria. Niger J Med 20(3): 360-365.
- Ojule J, Macpepple D (2011) Family Planning Practice in a Tertiary Health Institution in Southern Nigeria. West Afr J Med 30(3): 178-181.
- Bolarinwa O, Tessema Z, Frimpong J, Seidu A, Ahinkorah B (2021) Spatial distribution and factors associated with modern contraceptive use among women of reproductive age in Nigeria:A multilevel analysis. PLoS One 16(12): e0258844.
- Idowu A, Ukandu GC, Mattu J, Olawuyi D, Abiodun A, Adegboye P, et al. (2020) Modern Contraception: Uptake and Correlates among Women of Reproductive Age-Group in a Rural Community of Osun State, Nigeria. Ethiop J Health Sci 30(4): 531-540.
- Asresie MB, Fekadu GA, Dagnew GW (2020) Contraceptive use among women with no fertility intention in Ethiopia. PLoS One 15(6):1-13.
- Oyinlola FF, Bamiwuye SO, Adebowale SA, Ekundayo OO, Ilesanmi BB (2020) Variations in modern contraceptive uptake and its correlates in Southwest and Northeast Nigeria: a comparative analysis. Int J Reprod Contraception, Obstet Gynecol 9(7): 2852.
- Ononokpono DN, Odimegwu CO, Usoro NA (2020) Contraceptive use in Nigeria: Does social context matter? Afr J Reprod Health 24(1): 133-142.
- Ekholuenetale M, Olorunju S, Fowobaje KR, Onikan A, Tudeme G, et al. (2021) When Do Nigerian Women of Reproductive Age Initiate and What Factors Influence Their Contraceptive Use? A Contextual Analysis. Open Access J Contracept 12: 133-147.
- (2019) Department of Economic and Social Affairs United Nations. Contraceptive Use by Method pp. 1-15.
- Sanchez EK, McGuire C, Calhoun LM, Hainsworth G, Speizer IS (2021) Influences on contraceptive method choice among adolescent women across urban centers in Nigeria: a qualitative study. Contracept Reprod Med 6(1):1-10.
- Ebiogbo SO, Agbo J (2020) The pattern of reversible contraceptive uptake at the family planning and contraceptive unit at a tertiary hospital in Southern Nigeria. Yen Med J 2(2): 73-80.
- Crawford EE, Atchison CJ, Ajayi YP, Doyle AM (2021) Modern contraceptive use among unmarried girls aged 15-19 years in Southwestern Nigeria: results from a cross-sectional baseline survey for the Adolescent 360 (A360) impact evaluation. Reprod Health 18(1):1-13.
- Udigwe GO, Udigwe BI, Ikechebelu JI (2002) Contraceptive practice in a teaching hospital in south-east Nigeria. J Obstet Gynaecol (Lahore) 22(3): 308-311.
- Ahmed S, Choi Y, Rimon JG, Alzouma S, Gichangi P, et al. (2019) Trends in contraceptive prevalence rates in sub-Saharan Africa since the 2012 London Summit on Family Planning: results from repeated cross-sectional surveys. Lancet Glob Heal 7(7): e904-e911.
- Kamuyango A, Hou WH, Li CY (2020) Trends and contributing factors to contraceptive use in Kenya: A large population-based survey 1989 to 2014. Int J Environ Res Public Health 17(19): 1-12.
- Lasong J, Zhang Y, Gebremedhin SA, Opoku S, Abaidoo CS, et al. (2020) Determinants of modern contraceptive use among married women of sectional study reproductive age: a cross- in rural Zambia. BMJ Open 10(31): e030980.
- Diamond-Smith N, Logan R, Marshall C, Corbetta-Rastelli C, Gutierrez S, et al. (2021) COVID-19’s impact on contraception experiences: Exacerbation of structural inequities in women’s health. Contraception. 104(6): 600-605.
- Bello O, Agboola A (2020) Trends in contraceptive uptake at a tertiary health facility in Ibadan, Nigeria. Int J Med Heal Dev 25(1): 21.
- Kavanaugh ML, Pliskin E (2020) Use of contraception among reproductive-aged women in the United States, 2014 and 2016. F&S Reports 1(2): 83-93.
- Muhammad Z, Maimuna D (2014) Contraceptive trend in a tertiary facility in Northwestern Nigeria: A 10-year review. Niger J Basic Clin Sci 11(2): 99-103.
- Ossai AC, Jombo ES, Onwusulu DN, Fagbemi AJ, Ilikannu S (2021) Uptake of long-acting reversible contraception in federal medical centre, Asaba: A three year review. Int J Clin Obstet Gynaecol 5(5): 130-134.
- Akinloye O, Adediji I, Samuel TA, Popoola O, Iranloye BO, et al. (2022) Contraceptive Use among Women Assessing Family Planning Services in Different Levels of Health Care Facilities: A Decades Retrospective Review. J Community Med Public Heal Reports 3(05): 4-9.
- Wai MM, Bjertness E, Htay TT, Liabsuetrakul T, Myint ANM, et al. (2020) Dynamics of contraceptive use among married women in North and South Yangon, Myanmar: findings from a cross-sectional household survey. Contracept X 2: 100015.
- Ijarotimi A, Bakare B, Badejoko O, Fehintola A, et al. (2015) Contraceptive uptake among women attending family planning clinic in a Nigerian tertiary health facility: a 6-year review. Int J Reprod Contraception, Obstet Gynecol 4(3): 721-724.
- Anyatonwu OP, San Sebastián M (2022) Rural-urban disparities in postpartum contraceptive use among women in Nigeria: a Blinder-Oaxaca decomposition analysis. Int J Equity Health 21(1): 1-8.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...