Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6062
Research Article(ISSN: 2638-6062) 
Adjuvant use of Bromodihydrochlorophenylbenzodiazepine in Patients with Paranoid Schizophrenia with Ideator Pattern of Non- Suicidal Autoaggressive Behavior Volume 4 - Issue 5
Kravchenko IV1,2*, Chizhikov II2, Lvov NN2, Sidorov VG2, and Klevtsova EV2
- 1Interdistrict Center for Medical Rehabilitation at Polyclinic, St. Petersburg, Russia
- 2FKU “St. Petersburg Psychiatric Hospital of a Specialized Type with Intensive Observation”, St. Petersburg, Russia
Received: October 21, 2022; Published: November 09, 2022
*Corresponding author: Kravchenko IV, Interdistrict Center for Medical Rehabilitation at Polyclinic, St. Petersburg, Russia
DOI: 10.32474/PRJFGS.2022.04.000197
Abstract
The relevance of this work is due to the insufficient number of modern studies that reflect the principles of adjuvant use of benzodiazepine tranquilizers in the treatment of patients with paranoid schizophrenia with non-suicidal auto aggressive actions with neuroleptics. Purpose of the work: comparative analysis of the effectiveness of bromodihydrochlorophenylbenzodiazepine in patients with paranoid schizophrenia with an ideational pattern of non-suicidal auto-aggressive behavior. A total of 188 patients with paranoid schizophrenia who met the ICD-10 criteria were examined. The leading research method was clinical and psychopathological. The psychometric assessment of the clinical state was carried out using the scale of openly manifested aggression by Yudovsky, the scale of impulsivity by Pluchek, a brief evaluation of the psychiatric scale. Fisher’s test was used for statistical evaluation. Results. The adjuvant use of bromodihydrochlorophenylbenzodiazepine at the initial stage of therapy in the studied individuals made it possible to obtain more pronounced clinical effects due to their action of neuroleptics, especially haloperidol, in relation to impulsiveness and overt aggression. Conclusions: Adjuvant use of bromodihydrochlorophenibenzodiazepine in regimens with neuroleptics increases the effectiveness of therapy in relation to the leading psychopathological phenomena in patients with paranoid schizophrenia with the NSAB ideation pattern at the initial stage of therapy. In this case, preference should be given to antipsychotics with the most pronounced dopaminolytic effect (haloperidol).
Keywords: Paranoid schizophrenia; non-suicidal auto-aggression; antipsychotics, adjuvant use of tranquilizers; bromodihydrochlorophenyldibenzodiazepine
Introduction
Currently, the search for therapeutic schemes continues to enhance the effect of neuroleptic therapy in patients with schizophrenia. The solution of the problem is complicated by the increase in the proportion of behavioral disorders with aggressive and non-suicidal auto-aggressive actions, or “NSAA” for short [1,2]. One of the solutions to the stated problem is the adjuvant use of benzodiazepine tranquilizers [3]. Such drugs, being an allosteric modulator of GABAergic receptors, cause the opening of a chlorine-associated channel, followed by depolarization of the nerve cell and a decrease in its excitability. At the same time, drugs are able to have a central and peripheral effect, including at the level of the thalamus, hypothalamus, cerebellum, limbic system, basal ganglia, corpus callosum and other structures [4-9]. This pharmacodynamic profile allows the use of benzodiazepine tranquilizers in the treatment of schizophrenia spectrum disorders, including nonspecific psychomotor agitation, affective-delusional states, and anxiety-phobic disorders [10-13]. The lack of data on the use of benzodiazepine derivatives in patients with paranoid schizophrenia with NSAA determined the relevance of this study.
Purpose of the Study
Comparative analysis of the efficacy of bromodihydrochlorophenylbenzodiazepine in patients with paranoid schizophrenia with an ideational pattern of non-suicidal auto-aggressive behavior.
Materials and Methods
As part of a 6-week study, a continuous, non-randomized method was used to compare the effectiveness of monotherapy with selected antipsychotics and a regimen involving the adjuvant use of bromodihydrochlorophenyldibenzodiazepine. A total of 188 patients with paranoid schizophrenia with a continuously progressive type of course, an increasing tonic-type defect, and an ideation pattern of non-suicidal auto-aggressive behavior (abbr. NAAB) were examined. All patients were under long-term inpatient (compulsory) treatment in the St. Petersburg Specialized Psychiatric Hospital with intensive observation from 2009 to 2022. All subjects were men aged 20 to 55 years. The average age of the subjects was 29.4 ± 1.2 years. The average duration of a procedural disease was 16.1 ± 1.3 years. The inclusion criteria were: 1) compliance of the diagnosis of paranoid schizophrenia with the criteria of the ICD- 10 revision (F20.0); 2) the state of drug remission, with signs of an increasing procedural personality defect; 3) the implementation of NSAA by patients with paranoid schizophrenia at the time of being on inpatient compulsory treatment. Exclusion criteria were: 1) psychotic level of disorders prior to inclusion in the study; 2) auto-aggressive actions in the form of self-suffocation as a means of obtaining sexual satisfaction (asphyxiophilia); 3) taking the drugs declared for the study within a period of less than 6 months before the start of the study itself.
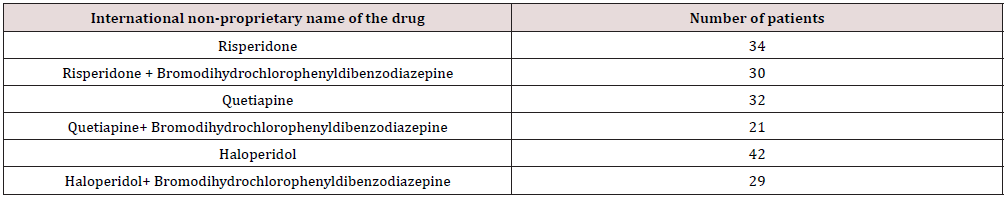
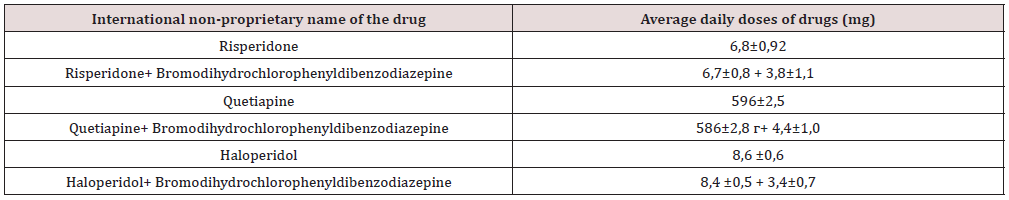
Remission meant “the weakening and mitigation of all symptoms, providing to some extent the social and labor adaptation of the patient, and embracing a wide range of conditions from those bordering on practical recovery to those in which the symptoms of the defect are already clearly visible” [14]. A schizophrenic defect, or in the modern interpretation, neurocognitive process changes, was understood as “such consequences of a mental illness that occur in conditions of a complete stop of the process, lead to a persistent (and not progressive) loss or dissociation of mental functions with a change in personality and are accompanied by a decrease in its functioning” [15]. Under the definition of “NSAA” fell a variety of actions directed against one’s health and accompanied by a violation of the integrity (functions) of organs or organ systems. At the same time, there was not any demonstration of the intention to commit suicide [16]. All patients were randomly distributed into 6 groups (Table 1). The choice of drugs corresponded to the principle of their greatest distribution in practical work. The choice of dosages of drugs in the examined persons was carried out taking into account the severity of clinical and psychopathological experiences (Table 2).
The development of the disease followed the classical path and included
a) A prodromal period.
b) The period of increasing manifestations of the activity of the process.
c) The period of the full development of the disease coincides with the period of the appearance of psychotic symptoms.
d) The stage of the formation of remission against the background of a decrease in the severity of psychotic experiences of an increase in deficient personality changes.
Retrospectively, the beginning of the prodromal period in paranoid schizophrenia in the examined individuals can be considered adolescence (13.2 ± 0.7 years), at which causeless mood swings, transient episodes of anxiety, followed by irritability and conflict, opposition to the immediate environment appeared. Decreased school performance. There were cases of dissatisfaction with appearance, episodes of eating disorders. The duration of this period averaged 2.1 ± 0.3 years. During the period of increasing manifestations of the activity of the schizophrenic process, affective and behavioral disorders increased. Patients experienced causeless sadness, depression, increased anxiety, opposition, conflict. By this period, patients significantly reduced their social activity, stopped attending educational institutions, and limited their social circle. Cases of aggressive and auto-aggressive behavior (both suicidal and non-suicidal) became more frequent. There were transient deceptions of perception, psychic automatisms (someone called by name, they felt a sense of accomplishment, the violence of their thoughts). The duration of the period averaged 0.7 ± 0.1 years.
The period of full development of the disease was characterized by detailed pictures of the delusional perception of the surrounding world. There were ideas of relationship, persecution, influence, auditory perceptual deceptions of an imperative nature, mental automatisms. A distinctive feature of the latter was the limitation of their manifestations to an exclusively ideatory variant. All patients in the acute period had episodes of psychomotor agitation, aggression towards others. Moreover, in 34% of the subjects, aggression was transformed into a primary initial delict, or the socalled “Paragnomen” phenomenon [17]. Thinking was inconsistent, with multiple atactic slips, shperrungs, and the phenomenon of mentism. Going into remission was of a lytic nature. At first, psychomotor agitation was reduced, then the affective charge of delusional ideas and the loss of the imperativeness of auditory hallucinations decreased. Emotional coldness, apato-abulic disorders came to the fore, while maintaining conflict, aggression against the background of a lack of criticism of the disease.
These changes led to a decrease in adaptive-compensatory functions, the manifestation of which was the infliction of nonsuicidal self-harm under conditions of making demands that were unbearable for a personality altered by the disease. This was most fully manifested when such patients were on inpatient (compulsory) treatment, when, in fact, for the first time in their lives they were forced to take neuroleptic therapy for a long time. Such patients were distinguished by increased subordination, fatigue, easily accepted requirements to comply with the criminal hierarchy of values and were not its active adherents. Communication with others was built on a formal basis, serving to satisfy the simplest everyday needs. Similarly, many authors describe the clinical picture of a growing personality defect of the asthenic, apato-abulic type, or, in the modern interpretation, deficient changes in the tonic level [18]. Actually, NSAA were considered in the structure of behavioral (psychopathic) forms of response and met the following criteria. next. In a number of cases, various external (psychogenic) factors acted as a trigger for the application of NSAA, for example, the need to comply with the requirements of the regime of detention, involvement in more active participation in rehabilitation activities. This group was joined by cases of harassment by physically stronger patients with criminal attitude behavior.
While maintaining an impulsive nature at the last stages of implementation, at the initial stage of planning, the subjects willingly discussed the preparation for the implementation of NSAA with other patients, choosing the least traumatic way of their implementation. The subsequent NSAAs were carried out according to the principle of the “last straw”, largely relieving the affective tension of the patients. Later, NSAA formed a protest model of response that was stable in time in the conditions of making demands on the individual, being pseudo-adaptive coping strategies. In some patients, non-suicidal self-harm was autochthonous in nature. In this case, NSAA was accompanied by short-term changes in the mental state, in which asthenia, apathy, disorganization of thinking, irritability, conflict, sleep disturbances increased for a period of two to three weeks, and protopathic anxiety appeared. In the available literature, such states are closest to the cases described by D.E. Melekhov (1964) of “episodic, shortterm, inadequate situation, mood swings and activity.” In another part of the cases, NSAA were retrospectively regarded as harbingers of exacerbation of psychotic symptoms, before which mood swings with depressed affect, anxiety, negativism, and sleep disturbances increased.
The NSAA themselves were carried out once, impulsively, with a formal critical assessment of their behavior. Thus, the ideator pattern of NSSB was characterized by negative disorders of the type of deficient changes in the tonic level with the presence of a formalized preparatory period before NSAA, their one-time nature, and formal criticism of one’s behavior. The assessment of the mental state of the examination was carried out by a clinical method at the time of inclusion in the study (1 week), then at 3 and 6 weeks of the study. The clinical efficacy of therapy was determined by a comparative analysis of the frequency of exacerbation of psychotic symptoms and committed acts of non-suicidal auto-aggression for a period of 24 weeks before and after inclusion in the study. To objectify the data obtained, the scale of openly manifested aggression by Yudovsky, the Pluchek impulsiveness scale, and the brief psychiatric assessment scale were used. Fisher’s test was used for statistical evaluation.
Virtual Autopsy
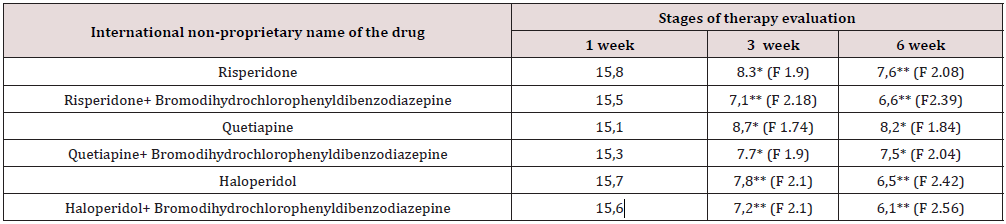
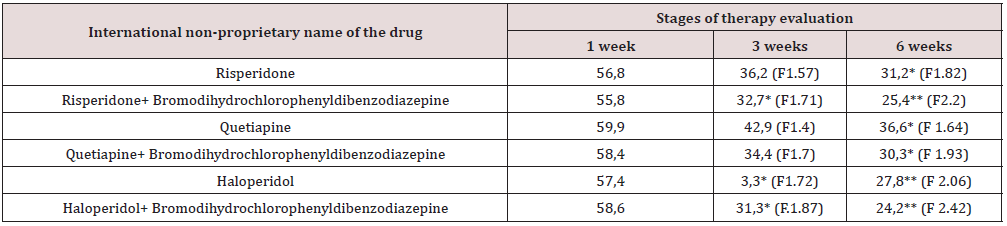
All antipsychotics declared in the study, both as monotherapy and in combination with bromodihydrochlorophenylbenzodiazepine, showed a positive effect on overt aggression (Table 3). Statistically significant changes in all examined patients on this scale occurred at the 3rd week of the study. At the same time, in patients who received adjuvant therapy with risperidone and haloperidol, as well as haloperidol monotherapy, statistically significant changes exceeded those in other patients. By the 6th week of the study, all patients in the study had positive statistically significant changes on the indicated scale. It was established that all antipsychotics declared in the study, both as monotherapy and with adjuvant use of bromodihydrochlorophenylbenzodiazepine, showed a positive effect on impulsivity (Table 4). Statistically significant changes in the impulsivity scale in patients taking adjuvant therapy with risperidone and haloperidol, as well as with haloperidol monotherapy, occurred in week 3 of the study. In other comparison groups, changes on this scale for 3 weeks of the study were noted at the level of trends.
*p<0,05; **p<0,01
*p<0,05; ** p<0,01
Statistically significant changes on this scale in all examined patients occurred in the 6th week of the study. At the same time, in patients taking adjuvant risperidone and haloperidol, as well as in monotherapy with haloperidol, statistically significant changes exceeded those in other patients. It was established that all antipsychotics declared in the study, both as monotherapy and with adjuvant use of bromodihydrochlorophenylbenzodiazepine, showed a positive effect on the general mental state (Table 5). It was found that statistically significant changes in the Brief Psychiatric Rating Scale in patients taking adjuvant therapy with risperidone and haloperidol, as well as with haloperidol monotherapy, occurred at week 3 of the study. In other comparison groups, changes on this scale for 3 weeks of the study were noted at the level of trends. Statistically significant changes on this scale in all examined patients occurred in the 6th week of the study. At the same time, in patients taking adjuvant risperidone and haloperidol, as well as in monotherapy with haloperidol, statistically significant changes exceeded those in other patients.
*p<0,05
Summarizing the results of the study, we can note the ability of bromodihydrochloropheylbenzodiazepine to potentiate the action of neuroleptics in the examined patients at the initial stage of therapy. It has been established that all neuroleptics used (risperidone, quetiapine, haloperidol) are effective against overt aggression. Adjuvant use of bromodihydrochlorophenibenzodiazepine changed the completeness of the clinical response in relation to overtly detectable aggressive urges. In particular, the adjuvant use of bromodihydrochlorophenylbenzodiazepine in a regimen with risperidone and haloperidol appeared to be more effective in relation to overtly detectable aggression in the examined patients; Adjuvant use of bromodihydrochlorophenylbenzodiazepine in the scheme with risperidone and haloperidol was more effective in relation to impulsivity in this group of patients; Finally, the adjuvant use of bromodihydrochlorophenylbenzodiazepine in a regimen with risperidone and haloperidol was more effective in terms of the overall change in mental state in the subjects we examined. Also noteworthy is the fact that atypical antipsychotics in the framework of monotherapy, as well as in combination treatment, were used in dosages close to the maximum daily. The dosage of bromodihydrochlorophenylbenzodiazepine approached the recommended daily average. At the same time, haloperidol, on the contrary, was used in relation to the same clinical targets in small daily dosages, which indicates its hidden clinical potential.
The theoretical substantiation of the obtained results can be the following
a) The pathogenetic basis of the leading clinical manifestations in the examined individuals is pathological dopaminergic activity in the area of the mesolimbicmesocortical tract.
b) Bromodihydrochlorophenylbenzodiazepine is an allosteric modulator for the gamma-aminobutyric acid receptor. The drug causes a reduction in excitatory neurotransmission, including norepinephrine, dopamine.
c) The clinical efficacy of bromodihydrochlorophenylbenzodiazepine is complemented by synergism with antipsychotic drugs, especially with a pronounced dopaminolytic effect (haloperidol).
The established clinical profile opens up the possibility of a wider use of bromodihydrochlorophenylbenzodiazepine as an adjuvant for a variety of autochthonous fluctuations in the mental state in patients with schizophrenia spectrum disorders. The results are preliminary and should include data on the impact on the negative spectrum of disorders, as well as the tolerability and safety of therapy. As a promising direction, the possibility of using in such patients, as adjuvant agents, other drugs with a pharmacodynamic profile similar to bromodihydrochlorophenylbenzodiazepine (for example, pregabalin) should be considered.
Virtual Autopsy Tools
Adjuvant use of bromodihydrochlorophenibenzodiazepine in regimens with neuroleptics increases the effectiveness of therapy in relation to leading psychopathological phenomena in patients with paranoid schizophrenia with the NSAB ideation pattern at the initial stage of therapy. In this case, preference should be given to antipsychotics with the most pronounced dopaminolytic effect (for example, haloperidol).
Conflict of Interests
No.
References
- Kravchenko IV (2016) A short guide to psychiatry. SpetsLit Publishers, Saint Petersburg, USA.
- Kravchenko IV, Chizhikov II, Lvov NN, Sidorov VG, Klevtsova EV (2022) Comparative analysis of the effectiveness of neuroleptics in patients with paranoid schizophrenia with a tonic type of defect and non-suicidal auto-aggressive actions who are under compulsory treatment. Social and Clinical Psychiatry 32(2): 53-58.
- Vorob'eva OV (2015) Benzodiazepines from skepticism to a rational (weighted) position. Psychiatry and psychopharmacotherapy 17(4): 19-24.
- Maskell PD, De Paoli G, Nitin Seetohul L, Pounder DJ (2012) Phenazepam: the drug that came in from the cold. J Forensic Leg Med 19(3): 122-125.
- Manchester KR, Lomas EC, Waters L, Dempsey FC, Maskell PD (2018) The emergence of new psychoactive substance (NPS) benzodiazepines: A review. Drug Test Anal 10(1): 37-53.
- Hofmann JI, Schwarz C, Rudolph U, Antkowiak B (2019) Effects of diazepam on low-frequency and high-frequency electrocortical γ-power mediated by α1- and α2-GABA(A) receptors. Int J Mol Sci 20(14): 3486.
- Khalid S, Rasool MF, Imran I, Abdul M, Hamid S, et al. (2021) A physiologically based pharmacokinetic model for predicting diazepam pharmacokinetics after intravenous, oral, intranasal, and rectal applications. Pharmaceutics 13(9): 1480.
- Mckillop LE, Fisher SP, Milinski L, Krone LB, Vyazovskiy VV (2021) Diazepam effects on local cortical neural activity during sleep in mice. Biochem Pharmacol 191: 114515.
- Burkat PM (2022) Physiologically Based Pharmacokinetic and Pharmacodynamic Modeling of Diazepam: Unbound Interstitial Brain Concentrations Correspond to Clinical End Points. J Clin Pharmacol 62(10): 1297-1309.
- Lejeune J, Larmo I, Chrzanowski W, Witte R, Karavatos A, et al. (2004) Oral risperidone plus oral lorazepam versus standard care with intramuscular conventional neuroleptics in the initial phase of treating individuals with acute psychosis. Int Clin Psychopharmacol 19(5): 259-269.
- Dold M, Li C, Tardy M, Khorsand V, Gillies D, et al. (2012) Benzodiazepines for schizophrenia. Cochrane Database Syst Rev 11(11): CD006391.
- Ostinelli EG, Hussein M, Ahmed U, Rehman FU, Miramontes K, et al. (2018) Risperidone for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev 4(4): CD009412.
- Krasnov V (2018) Smulevich A.B. Lights schizophrenia and borderline states. M, 2017. Review of book. Psychiatry 1(77): 144-145.
- Zenevich GV (1964) Remission in schizophrenia. Leningrad: Medicine Publishers.
- Melekhov DE (1963) Clinical basis for assessing performance in schizophrenia. -Moscow: Medgiz. Publishers.
- Nock MK, Favazza AR (2009) Nonsuicidal self-injury: Definition and classification.
- Jagoda Z, Maslowski J (1965) List of publications of Eugeniusz Brzezicki [Bibliography of works of Eugeniusz Brzezicki] Neurol Neurochir Psychiatr Pol 15(4): 533-542.
- Neznanov NG, Ivanov MV (2021) Negative and cognitive disorders in endogenous psychoses: diagnostics, clinic, therapy. Moscow: MEDpress-inform Publishers, USA.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...